When you’re on a proton pump inhibitor (PPI) for heartburn and suddenly need an antifungal for a stubborn yeast infection, things get complicated-fast. These two types of drugs don’t just sit quietly in your body. They bump into each other in ways that can make one or both fail. And it’s not just a theoretical concern. In 2023, nearly 1 in 5 hospitalized patients in the U.S. got both a PPI and an antifungal at the same time. That’s over 400,000 people a month. Many of them didn’t get the full benefit of their antifungal treatment because of a simple, avoidable interaction.
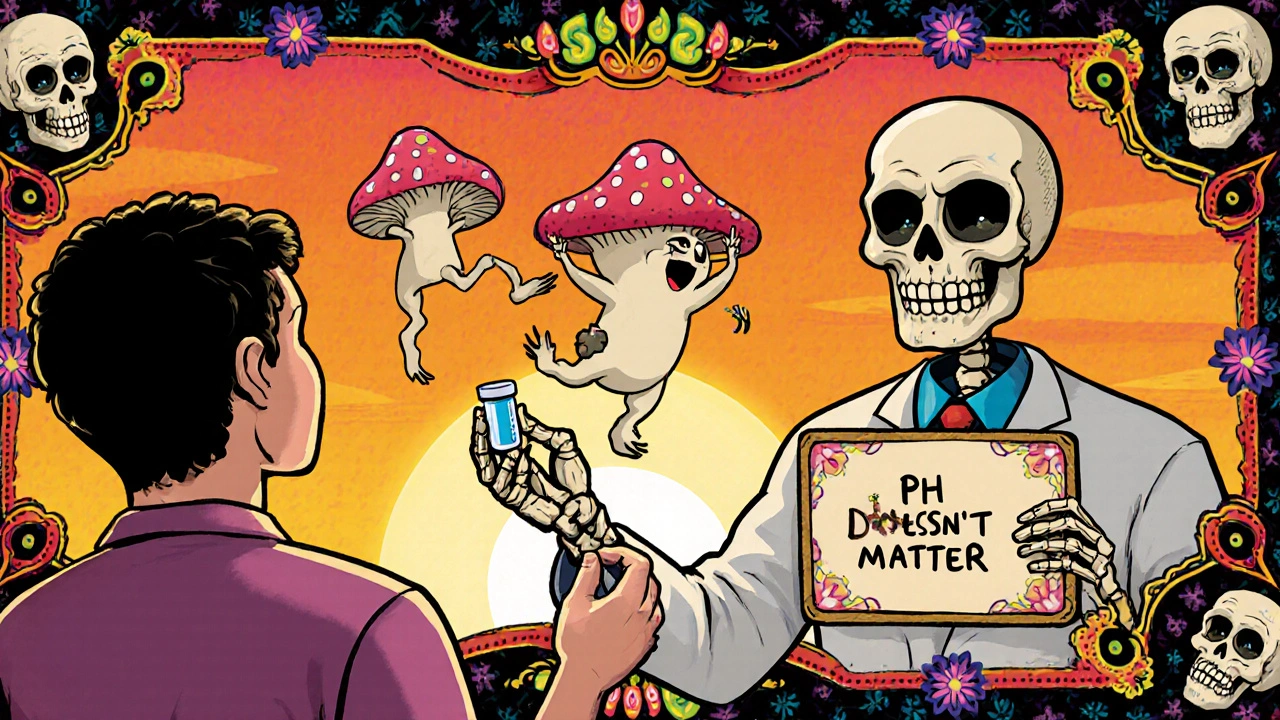
Why Your Antifungal Might Not Work With a PPI
Proton pump inhibitors like omeprazole, esomeprazole, and pantoprazole work by shutting down stomach acid production. That’s great for reducing acid reflux, but it’s terrible for certain antifungals. The problem? Some antifungals need acid to dissolve properly before they can be absorbed into your bloodstream. Without enough acid, they just pass through your gut like invisible pills.
Take itraconazole and ketoconazole. These are powerful antifungals used for serious fungal infections. But their solubility drops off a cliff when stomach pH rises above 4. Studies show that when taken with a PPI, their absorption drops by up to 60%. That means your blood levels of the drug might fall below the minimum needed to kill the fungus. The FDA added a black box warning to itraconazole’s label in 2023 because of this. It’s not a suggestion-it’s a red flag.
Fluconazole, on the other hand, doesn’t care. It’s highly water-soluble and absorbs just fine regardless of stomach pH. Its bioavailability stays around 90% even if you’ve taken a PPI an hour before. That’s why many pharmacists switch patients from itraconazole to fluconazole when a PPI is needed. Simple swap. Big difference.
The Hidden Twist: PPIs Might Actually Help Antifungals
Here’s where it gets weird. While PPIs hurt absorption of some antifungals, they might actually make them stronger inside your body. A 2024 study published in PMC10831725 found something unexpected: omeprazole, the most common PPI, directly interferes with a fungal enzyme called Pam1p-a proton pump on the surface of Candida cells. This enzyme helps the fungus survive in acidic environments and resist antifungal drugs.
When omeprazole blocks Pam1p, it weakens the fungus. In lab tests, fluconazole became 4 to 8 times more potent against resistant Candida glabrata strains when combined with omeprazole. That’s not a small effect. It’s like turning a weak flashlight into a spotlight. This discovery is so surprising that Johns Hopkins is now running a Phase II trial (NCT05876543) to see if adding omeprazole to standard fluconazole therapy can treat stubborn, drug-resistant yeast infections.
So here’s the paradox: PPIs reduce how much antifungal gets into your blood, but once it’s there, the PPI helps it work better. For fluconazole, this might balance out. For itraconazole, the absorption loss is so severe that even enhanced potency doesn’t help. You can’t kill a fungus if you don’t have enough drug in your system.
Which Antifungals Are Safe With PPIs? Here’s the Breakdown
Not all antifungals react the same way. Here’s what the data shows:
| Antifungal | Absorption Affected by PPIs? | Metabolic Interaction with CYP Enzymes? | Clinical Recommendation |
|---|---|---|---|
| Itraconazole | Yes - up to 60% reduction in blood levels | Yes - metabolized by CYP3A4 | Contraindicated. Use alternative antifungal. |
| Ketoconazole | Yes - absorption drops sharply above pH 4 | Yes - CYP3A4 substrate | Avoid entirely with PPIs. Rarely used today. |
| Fluconazole | No - unaffected by gastric pH | Yes - inhibits CYP2C9 and CYP3A4 at higher doses | Safe for absorption. Watch for drug interactions with blood thinners. |
| Voriconazole | Minimal impact | Yes - metabolized by CYP2C19 and CYP3A4 | Monitor blood levels. PPIs may reduce clearance by 25-35%. |
| Echinocandins (e.g., caspofungin) | No - IV only, no GI absorption | No - not metabolized by liver enzymes | Preferred choice when PPIs are needed. |
Notice that echinocandins-given intravenously-don’t interact at all. That’s why 87% of infectious disease pharmacists surveyed in 2023 preferred switching to an echinocandin rather than trying to manage the interaction. It’s simpler, safer, and more reliable.
What Happens If You Take Them Together Anyway?
Let’s say you’re on omeprazole for chronic reflux and get diagnosed with a fungal infection. Your doctor prescribes itraconazole. You take them together because you forgot to ask about timing. What happens?
Within days, your blood levels of itraconazole drop below 0.5 μg/mL-the minimum needed to suppress fungal growth. The infection doesn’t get better. Maybe it gets worse. You come back to the clinic. Your doctor thinks the drug didn’t work, so they increase the dose. Now you’re on a higher dose, which increases your risk of liver damage and heart rhythm problems. Meanwhile, your reflux is still being treated, so the absorption issue continues. You’re stuck in a cycle of failed treatment and rising side effects.
This isn’t hypothetical. A 2024 audit by the Institute for Safe Medication Practices found that over 22% of itraconazole prescriptions in community pharmacies were still being filled with a PPI. That’s more than 1 in 5 patients. Many of these patients didn’t even know they were at risk.
How to Manage This Interaction Safely
If you absolutely need both a PPI and a pH-dependent antifungal, timing matters-but it’s not a perfect fix.
- Itraconazole: Take it at least 2 hours before your PPI. Some studies show this reduces absorption loss from 60% to 45%. Still risky, but better than nothing.
- Ketoconazole: Don’t take it with a PPI. Period. There’s no safe workaround.
- Voriconazole: Get a blood test 72 hours after starting the PPI. Your dose may need to be lowered by 25-50% to avoid toxicity.
- Fluconazole: No timing needed. Just be aware it can make blood thinners like warfarin stronger. Your INR should be checked if you’re on both.
Many hospitals now have protocols. UCSF requires therapeutic drug monitoring for itraconazole if used with a PPI. Mayo Clinic recommends separating doses by 4-6 hours. Cleveland Clinic checks voriconazole levels within 3 days of adding a PPI. These aren’t suggestions-they’re standard care.

What’s Coming Next?
The future is changing. Researchers are developing new versions of itraconazole that don’t need stomach acid to work. One formulation, called SUBA-itraconazole, uses tiny particles that dissolve even in neutral pH. A 2023 Phase I trial showed 92% bioavailability regardless of whether the patient took a PPI. That’s a game-changer.
Meanwhile, the idea of using PPIs as antifungal boosters is gaining traction. If proven in clinical trials, we could start using low-dose omeprazole not just for heartburn-but as part of antifungal therapy for resistant infections. Imagine treating a stubborn yeast infection with a $5 generic pill and a standard antifungal. That’s the promise.
For now, though, the message is clear: don’t mix itraconazole or ketoconazole with PPIs. If you’re on a PPI and need an antifungal, ask your doctor or pharmacist: "Is this one affected by stomach acid?" If the answer is yes, there’s almost always a better option.
Bottom Line
Proton pump inhibitors and antifungals don’t play well together-but not all antifungals are created equal. Itraconazole and ketoconazole are vulnerable. Fluconazole and echinocandins are safe. And the newest research suggests that PPIs might one day help antifungals work better, not worse. But that’s still experimental.
Right now, the safest move is simple: know which antifungal you’re taking. If it’s itraconazole, don’t take it with a PPI. If you’re on a PPI and need an antifungal, ask for fluconazole or an echinocandin. And if you’re unsure, talk to your pharmacist. They’re trained to catch these hidden interactions before they hurt you.








8 Comments
Danny Nicholls November 23, 2025
OMG I just realized I was taking omeprazole with itraconazole last year 😳 my yeast infection never went away and I thought I was just "really bad at healing"... turns out I was just dumb. Thanks for this post, saved me from future dumb mistakes. Also 🙏
manish chaturvedi November 24, 2025
Thank you for this comprehensive overview. In India, many patients self-medicate with antifungals and proton pump inhibitors without consulting a pharmacist. This kind of clarity can prevent serious therapeutic failures. The table is especially helpful for clinical practice.
Nikhil Chaurasia November 25, 2025
It’s... it’s just so tragic. Here we are, with all this modern science, and people are still getting sicker because of something as simple as timing. I mean, how many lives have been lost to this? How many people are still being told "it’s in your head" when really, it’s just a drug interaction nobody bothered to check? My heart aches.
Holly Schumacher November 26, 2025
Actually, you missed a critical point: fluconazole’s inhibition of CYP2C9 and CYP3A4 can cause life-threatening bleeding when combined with warfarin. You mentioned it in passing, but this isn’t a footnote-it’s a black box warning-level interaction. And you didn’t even address the fact that voriconazole levels are wildly variable in CYP2C19 poor metabolizers, which is 15-20% of Asians. This post is dangerously incomplete.
Michael Fitzpatrick November 28, 2025
Man, I love how medicine keeps surprising us. Like, here we thought PPIs were just acid blockers, and now it turns out they’re kinda secretly helping antifungals fight back against resistant fungi? That’s wild. I mean, imagine if we started prescribing omeprazole as a booster for stubborn yeast infections-it’s like giving your body a secret weapon. And honestly, the idea of SUBA-itraconazole sounds like something out of sci-fi. I’m just glad we’re moving toward smarter, more targeted treatments instead of just throwing pills at problems.
Shawn Daughhetee November 28, 2025
i had a friend who got prescribed itraconazole and was on pantoprazole and her infection got worse and her doc just upped the dose and she ended up in the er with liver issues. this needs to be shouted from the rooftops
Miruna Alexandru November 30, 2025
It’s fascinating how we’ve constructed a medical paradigm where we treat symptoms (acid reflux) with a drug that inadvertently undermines another critical therapeutic intervention (antifungal efficacy). This isn’t just a pharmacokinetic quirk-it’s a systemic failure of reductionist thinking. We optimize one variable and collapse the entire system. The fact that we’re now considering PPIs as adjuvant antifungals only deepens the irony: we’re weaponizing the very mechanism we previously pathologized. Are we healing, or just rearranging the chaos?
Justin Daniel December 1, 2025
So basically… if you’re on a PPI and need an antifungal, just ask your pharmacist: "Is this one the type that needs stomach acid to work?" If they hesitate? Run. Or better yet, ask for fluconazole or an IV one. Simple. No drama. No guesswork. And hey-if you’re the kind of person who takes omeprazole like candy because "it helps with bloating," maybe… just maybe… talk to someone about why you’re so uncomfortable with your own digestion. Just saying. 😊