Asthma Management: Practical Steps to Keep Your Lungs Happy
If you’ve ever felt short of breath during a simple walk, you know asthma can ruin everyday moments. The good news? Most flare‑ups are preventable with a few smart habits. Below are hands‑on tips you can start using right now.
Master Your Inhaler Technique
The most common mistake isn’t the medication—it’s how it’s taken. For a metered‑dose inhaler (MDI), shake it, breathe out fully, then place the mouthpiece between your teeth and lips. Press the canister while starting a slow inhale, hold for about ten seconds, and exhale gently. Spacer devices make this easier; they catch the spray so more medicine reaches your lungs.
Dry powder inhalers (DPIs) work differently—no shaking needed. Just load a dose, breathe in quickly and deeply, then hold your breath. If you’re unsure which type you have, ask your pharmacist for a quick demo. Practicing daily, even when you feel fine, ensures the technique sticks.
Identify and Dodge Triggers
Asthma loves anything that irritates the airways: pollen, pet dander, smoke, strong smells, even cold air. Keep a simple diary for a week—note when symptoms flare and what you were doing. Patterns will pop up quickly.
Once you know your triggers, take concrete steps: use HEPA filters at home, wash bedding in hot water weekly, keep windows closed on high‑pollen days, and avoid vaping or smoking areas. If cold air bites, wear a scarf over your nose and mouth during winter walks; the warmed air is gentler on bronchial tubes.
For outdoor enthusiasts, an inhaler should always be within arm’s reach—preferably in a pocket‑size holder you can clip to a belt or backpack. If you’re traveling, pack extra doses in your carry‑on and keep them away from extreme temperatures.
Build a Lifestyle That Supports Your Lungs
Regular exercise strengthens the muscles that help you breathe. Start with low‑impact activities like walking, swimming, or cycling for 20 minutes three times a week. Use a reliever inhaler before workouts if your doctor recommends it—this pre‑emptive step often prevents sudden coughing.
Stay hydrated. Thin mucus is easier to clear, so drink plenty of water throughout the day. A balanced diet rich in fruits, veggies, and omega‑3 fats can also reduce airway inflammation.
Don’t skip routine check‑ups. Your doctor may adjust dosages or suggest new controllers like inhaled steroids or leukotriene modifiers based on how you’ve been doing. Bring your symptom diary to the appointment; it makes medication tweaks faster and more accurate.
Finally, keep a written asthma action plan in an obvious spot—on the fridge, next to your meds, or saved on your phone. It should list daily medicines, signs that a flare‑up is starting, and when to use rescue inhalers versus calling emergency services.
Managing asthma isn’t about dramatic lifestyle overhauls; it’s about tiny, consistent actions that add up. Master the inhaler, know your triggers, stay active, and keep communication open with your healthcare team. Follow these steps and you’ll find yourself breathing easier, faster, and with far fewer interruptions.
- Archer Pennington
- 9
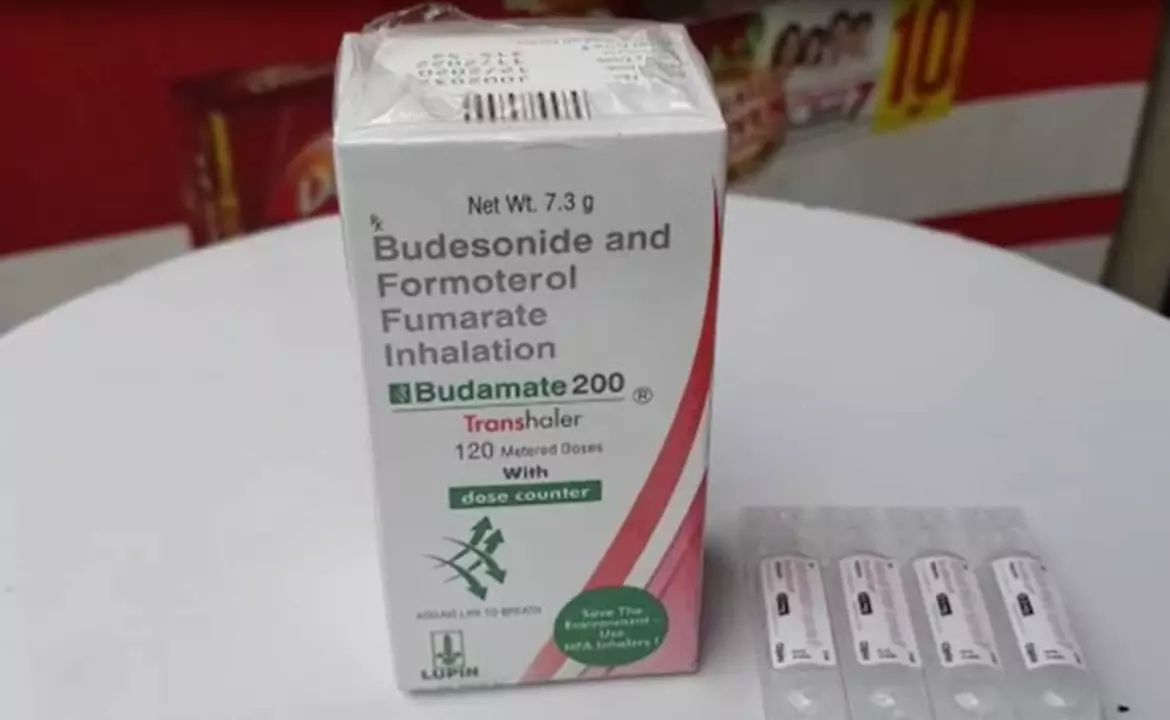
Budesonide formoterol and patient education: empowering patients for better asthma management
As a blogger, I cannot stress enough the importance of patient education in managing asthma effectively. A combination of Budesonide and Formoterol has proven to be a game-changer for many asthma sufferers. By understanding how these medications work and how to use them properly, patients can take control of their condition and improve their quality of life. I encourage everyone with asthma to learn more about Budesonide Formoterol and discuss it with their healthcare provider. Knowledge is power, and in this case, it could mean the difference between struggling with asthma and living a healthier, happier life.
Read more