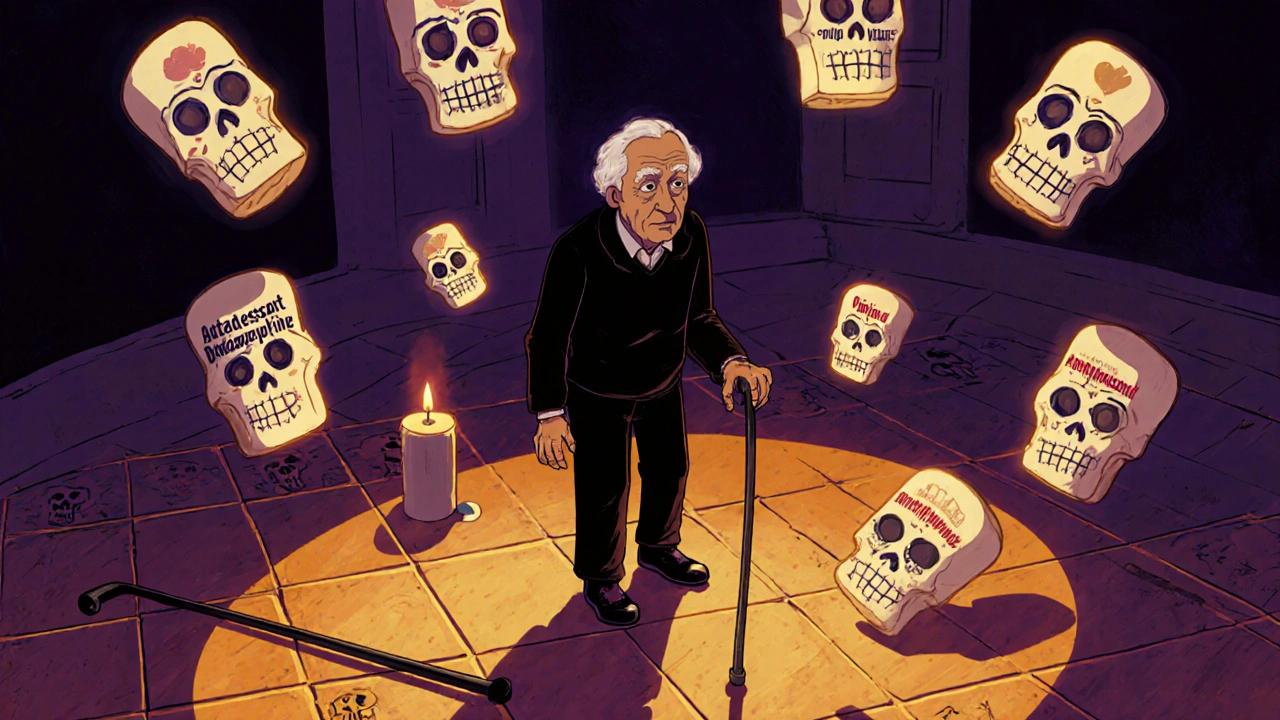
Beers Criteria: What Every Doctor and Caregiver Needs to Know
When you’re over 65, some common medicines can do more harm than good. That’s where the Beers Criteria, a regularly updated list of potentially inappropriate medications for older adults. Also known as the AGS Beers Criteria, it’s used by doctors, pharmacists, and nursing homes to cut down on risky prescriptions that can cause falls, confusion, kidney damage, or even death. It’s not a rulebook—it’s a safety net. And if you’re caring for an elderly parent or loved one, you need to understand it.
The Beers Criteria, a regularly updated list of potentially inappropriate medications for older adults. Also known as the AGS Beers Criteria, it’s used by doctors, pharmacists, and nursing homes to cut down on risky prescriptions that can cause falls, confusion, kidney damage, or even death. isn’t just about banning drugs. It’s about recognizing how aging changes the body. As we get older, our kidneys and liver don’t clear drugs the same way. That means even normal doses can build up to toxic levels. Drugs like benzodiazepines, anticholinergics, and certain painkillers are flagged because they’re linked to memory loss, dizziness, urinary retention, and worse. The criteria also warns against using multiple drugs at once—something called polypharmacy, the use of multiple medications by a patient, often leading to harmful interactions. Also known as multiple medication use, it’s one of the top reasons older adults end up in the ER. You’ll find posts here about proton pump inhibitors, tramadol, phenytoin, and citalopram—all drugs that show up on the Beers list for good reason. One study found that nearly 30% of nursing home residents were prescribed at least one Beers Criteria drug. That’s not normal. That’s preventable.
What makes the Beers Criteria powerful is that it’s based on real patient outcomes, not theory. It doesn’t just say "avoid this drug." It tells you why, and often, what to use instead. For example, instead of diphenhydramine for sleep, melatonin or behavioral changes are safer. Instead of long-acting benzodiazepines for anxiety, non-drug therapies or shorter-acting alternatives are recommended. The criteria also flags drugs that are fine for younger people but dangerous for seniors—like certain antihistamines, muscle relaxants, and even some antidepressants. And it’s not static. Every few years, experts review the latest research and update it. The 2023 version added new warnings for drugs like gabapentin and certain antipsychotics used off-label for dementia.
If you’re a caregiver, don’t wait for your doctor to bring it up. Ask: "Is this medication on the Beers Criteria list?" Bring a full list of all pills, vitamins, and supplements to every appointment. Watch for new symptoms—confusion, drowsiness, balance problems—that might be drug-related. The posts here cover real cases: how phenytoin levels can spike after a generic switch, why tramadol raises seizure risk in older adults, how SSRIs like citalopram can trigger mania in those with undiagnosed bipolar disorder. These aren’t abstract concerns. They’re daily risks in homes and nursing facilities across the country. The Beers Criteria isn’t about limiting care. It’s about making sure care doesn’t accidentally hurt the very people it’s meant to help.
- Archer Pennington
- 15
Falls and Medications: Which Drugs Increase Fall Risk for Seniors
Many seniors fall because of medications they’ve been taking for years. Learn which drugs-prescription and over-the-counter-increase fall risk, how they affect balance, and what you can do to reduce danger.
Read more