Deprescribing Seniors: Safe Ways to Reduce Unnecessary Medications
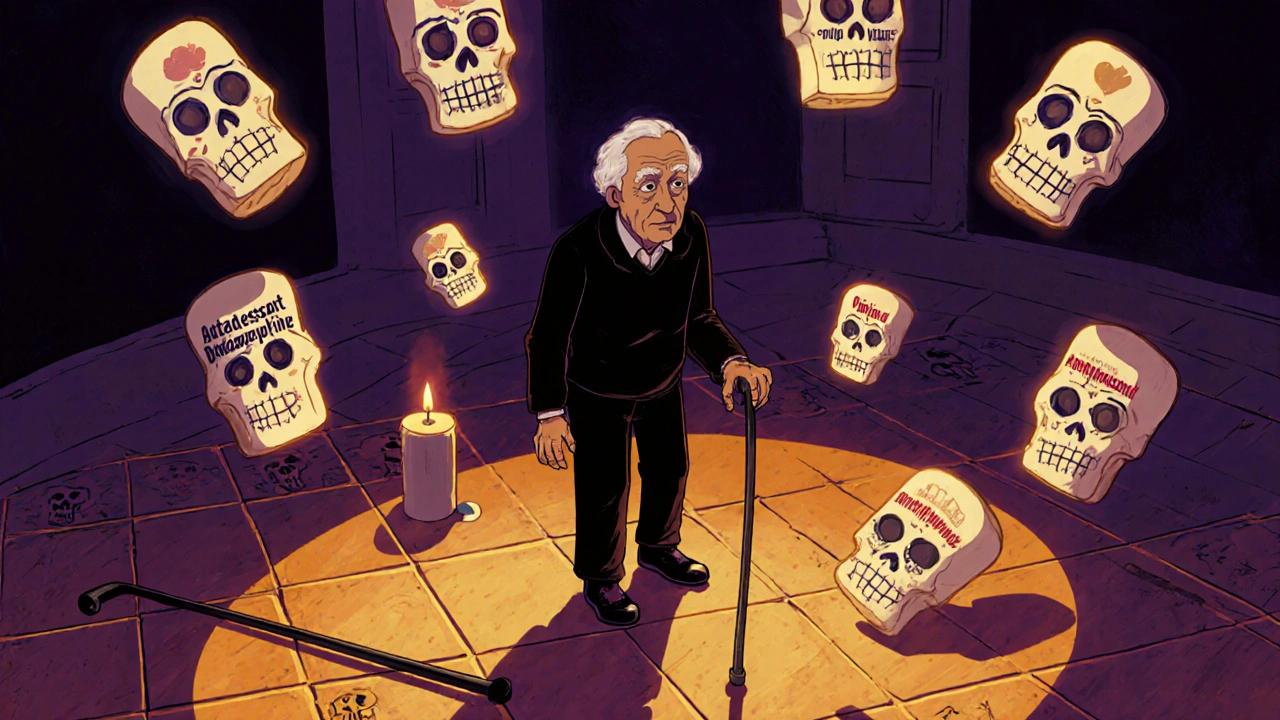
When we talk about deprescribing seniors, the process of carefully stopping or reducing medications that are no longer needed or may be harmful. Also known as medication reduction in older adults, it’s not about taking fewer pills just for the sake of it—it’s about removing drugs that don’t help anymore, cause side effects, or interact dangerously with others. Many seniors take five, ten, or even more medications daily. Some were prescribed years ago for conditions that have changed. Others were added to treat side effects from earlier drugs. This cycle, called polypharmacy in elderly, the use of multiple medications by older patients, often leading to increased risk of adverse reactions, isn’t always intentional. It’s often the result of fragmented care, missed follow-ups, or doctors focusing on one issue at a time without seeing the full picture.
Drug interactions, when two or more medications affect each other’s action in the body, sometimes dangerously are a huge concern in this group. For example, a proton pump inhibitor might weaken the effect of an antifungal, or a blood thinner could become too strong when mixed with turmeric supplements. These aren’t rare edge cases—they happen every day in nursing homes and clinics. And when a senior is on ten drugs, even one bad interaction can lead to falls, confusion, kidney damage, or hospitalization. That’s why geriatric pharmacology, the study of how medications affect older bodies differently than younger ones is so critical. Aging changes how the liver and kidneys process drugs. Muscle mass drops, fat increases, and the brain becomes more sensitive to sedatives. What was safe at 60 might be risky at 80.
Deprescribing isn’t about stopping everything. It’s about asking: Is this still helping? Could it be causing more harm? Are there simpler, safer options? Some seniors have been on sleeping pills for a decade. Others still take acid reflux meds they don’t need. A few even take statins after their heart risk has dropped to near zero. The goal isn’t to panic and quit cold turkey—it’s to work with a doctor to review each drug, one by one, with clear goals. Sometimes, stopping a drug leads to better sleep, clearer thinking, or fewer falls. Other times, it just removes a pill that’s doing nothing at all.
What you’ll find in the posts below are real, practical stories about how medications are being reevaluated in older adults. You’ll see how generic drugs can sometimes cause problems, how insurance coverage affects what people actually take, and how simple checks at the pharmacy can prevent dangerous mistakes. There’s no magic formula, but there are clear patterns—and the right questions can make all the difference.
- Archer Pennington
- 15
Falls and Medications: Which Drugs Increase Fall Risk for Seniors
Many seniors fall because of medications they’ve been taking for years. Learn which drugs-prescription and over-the-counter-increase fall risk, how they affect balance, and what you can do to reduce danger.
Read more