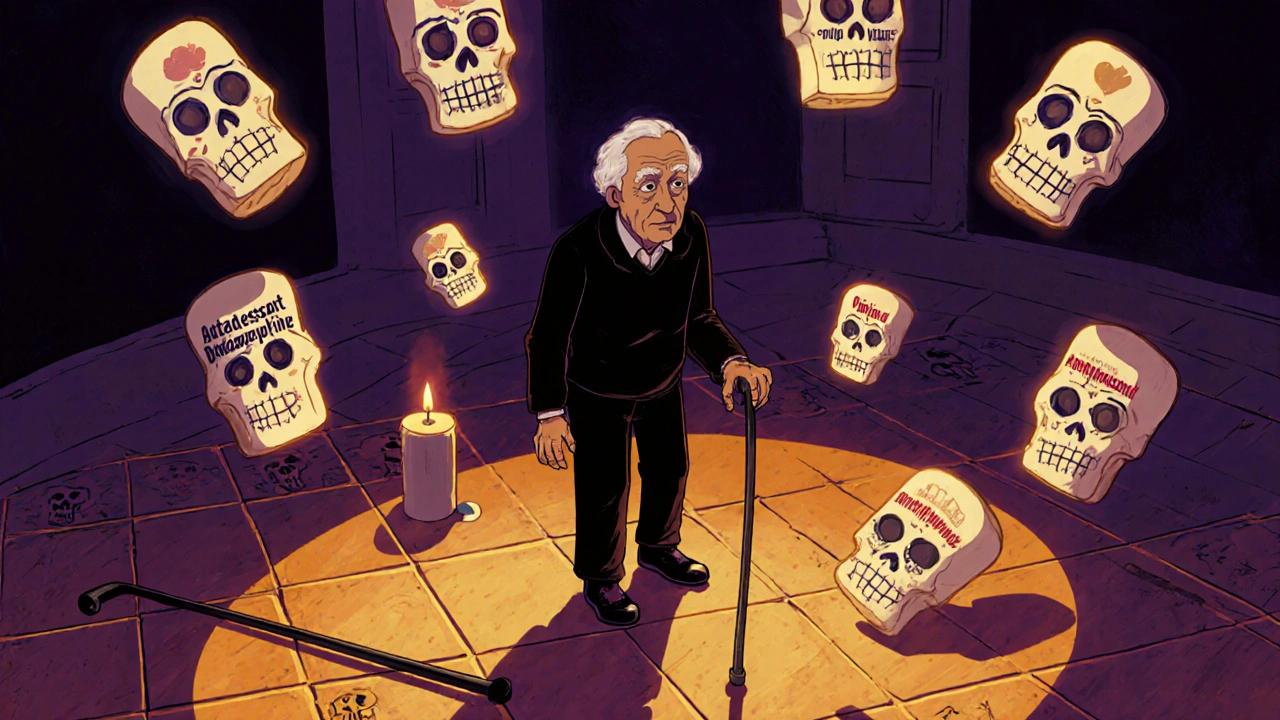
Medications That Cause Falls: What You Need to Know
When you take a pill to manage pain, anxiety, or high blood pressure, you might not think it could make you stumble. But medications that cause falls, drugs that impair balance, coordination, or alertness, leading to increased risk of falling. Also known as fall risk medications, these aren’t rare outliers—they’re common prescriptions many people take daily. The problem isn’t always the drug itself, but how it interacts with aging bodies, other pills, or even simple changes like standing up too fast.
Take benzodiazepines, sedatives used for anxiety and sleep, known to slow reaction time and cause dizziness. Drugs like diazepam or lorazepam are often prescribed for short-term use, but many people keep taking them for months or years. That’s when the risk spikes. Studies show older adults on these meds are up to 60% more likely to fall. Then there’s antihypertensives, blood pressure medications that can drop pressure too quickly, causing lightheadedness when standing. A sudden drop in blood pressure—called orthostatic hypotension—is a silent trigger for falls. Even common drugs like hydrochlorothiazide or lisinopril can do this, especially if you’re dehydrated or taking them at night.
It’s not just sedatives and blood pressure pills. antidepressants, especially SSRIs and tricyclics, can cause drowsiness, blurred vision, and low sodium levels, all of which mess with balance. Antipsychotics like quetiapine? Same story. Even over-the-counter sleep aids with diphenhydramine can leave you groggy and unsteady. And here’s the catch: these effects aren’t always obvious. You might not feel dizzy until you’re already halfway to the floor.
What makes this worse? Polypharmacy. Taking five, six, or more meds at once multiplies the risk. A pill that’s fine alone can become dangerous when stacked with another. That’s why checking your full list with your pharmacist isn’t just smart—it’s lifesaving. You don’t need to stop every med. But you do need to know which ones are pulling you down. Some drugs can be switched to safer alternatives. Doses can be lowered. Timing can be adjusted. Simple changes, like getting up slowly or adding night lights, help too.
This collection of articles dives into the real-world impact of these drugs. You’ll find clear breakdowns of which pills are most risky, how they affect your body, and what to ask your doctor. From how proton pump inhibitors quietly mess with nutrient absorption to why tramadol can trigger seizures and make you wobble, these posts cut through the noise. You’ll see how generic switches can be risky with drugs like phenytoin, and why even vitamin D supplements might not help if your real problem is a medication that’s pulling you off your feet. This isn’t about fear. It’s about control. You deserve to take what you need without putting yourself at risk.
- Archer Pennington
- 15
Falls and Medications: Which Drugs Increase Fall Risk for Seniors
Many seniors fall because of medications they’ve been taking for years. Learn which drugs-prescription and over-the-counter-increase fall risk, how they affect balance, and what you can do to reduce danger.
Read more