Senior Fall Risk: What Causes It and How to Prevent It
When an older adult falls, it’s not just a stumble—it’s a turning point. Senior fall risk, the likelihood that an older person will experience a fall due to physical, environmental, or medication-related factors. Also known as elderly fall risk, it’s one of the leading causes of injury, hospitalization, and loss of independence in people over 65. One in four seniors falls each year, and half of them don’t even tell their doctor. That’s not fear—it’s silence. And it’s deadly.
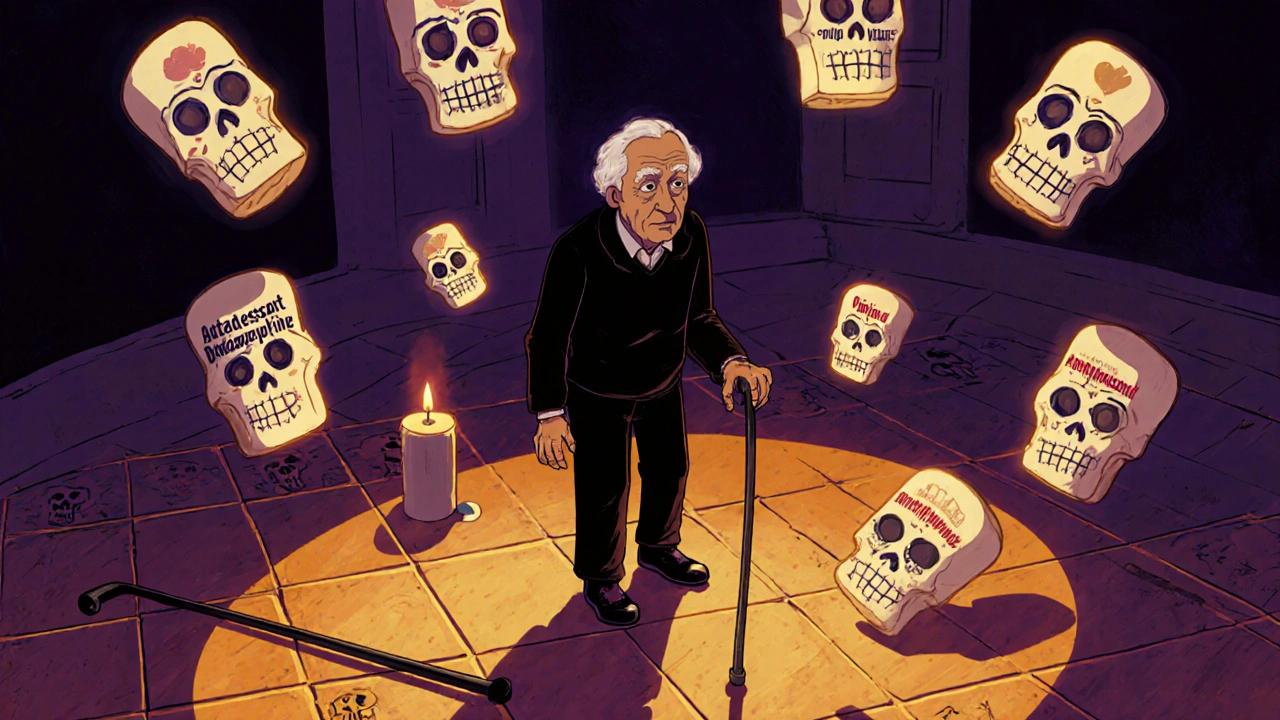
What makes someone more likely to fall? It’s rarely just one thing. Weak muscles, poor balance, vision problems, and slow reflexes all play a part. But here’s what most people miss: medication side effects in elderly, how certain drugs like sedatives, blood pressure pills, or antidepressants can throw off balance and coordination. A study from the CDC found that seniors taking four or more medications are twice as likely to fall. It’s not the pills themselves—it’s the combo. Proton pump inhibitors, antifungals, tramadol, even common blood pressure drugs like candesartan or perindopril can affect dizziness, muscle control, or alertness. And if you’re switching generics for phenytoin or adjusting insulin for travel, that tiny change can be enough to tip the scale.
Then there’s the environment. Loose rugs, dim lights, cluttered hallways—these aren’t just annoyances. They’re traps. But here’s the good news: most falls are preventable. Strength training, vision checks, home safety tweaks, and regular medication reviews with a pharmacist can cut fall risk by up to 30%. You don’t need fancy gadgets. You need awareness. You need to ask: Is this pill making me wobbly? Is my bathroom safe? Do I have someone to check on me?
And let’s not forget the hidden cost: fear. Once a senior falls—even once—they start avoiding movement. They stop walking, stop going out, stop living. That’s when weakness sets in, and the risk grows again. It’s a cycle. Breaking it starts with recognizing the signs: shuffling feet, holding onto furniture, saying "I’m just getting older." That’s not aging. That’s a warning.
Below, you’ll find real, practical advice from people who’ve been there. From how to verify your prescription to avoid dangerous mix-ups, to understanding how long-term care insurance covers—or doesn’t cover—medications that could be helping or hurting. You’ll see how vitamin D doesn’t fix statin pain, why tramadol can trigger seizures, and how generic switches can be risky with narrow-window drugs. These aren’t abstract theories. They’re the details that keep someone on their feet.
- Archer Pennington
- 15
Falls and Medications: Which Drugs Increase Fall Risk for Seniors
Many seniors fall because of medications they’ve been taking for years. Learn which drugs-prescription and over-the-counter-increase fall risk, how they affect balance, and what you can do to reduce danger.
Read more