When your kidneys suddenly stop working the way they should, it’s not just a lab result that changes-it’s your whole body. Acute Kidney Injury (AKI) doesn’t sneak up quietly. It hits fast. One day you feel fine; the next, you’re struggling to breathe, your legs are swollen, and your urine has dropped to almost nothing. This isn’t a slow decline. It’s a medical emergency that can turn deadly in hours if missed.
What Happens When Your Kidneys Shut Down
Your kidneys don’t just make urine. They filter toxins, balance electrolytes, control blood pressure, and keep your fluid levels stable. When AKI strikes, all of that collapses. The most common sign? Not enough urine. Less than 400 milliliters in 24 hours-that’s less than two soda cans. Some people stop peeing entirely. But here’s the twist: nearly one in five AKI cases show no symptoms at all. You feel fine. Your urine looks normal. Then a routine blood test reveals creatinine has jumped from 0.9 to 2.1. That’s a red flag.Other signs aren’t subtle. Fluid backs up into your lungs, making you gasp for air. Sodium and potassium go haywire. High potassium can stop your heart. Your blood gets acidic. You feel exhausted, nauseous, confused. In older adults, brain fog can look like dementia. Flank pain? That’s a clue it’s coming from inside the kidney itself. Chest pain? Could be inflammation around the heart. These aren’t random symptoms-they’re warning signs your body is drowning in its own waste.
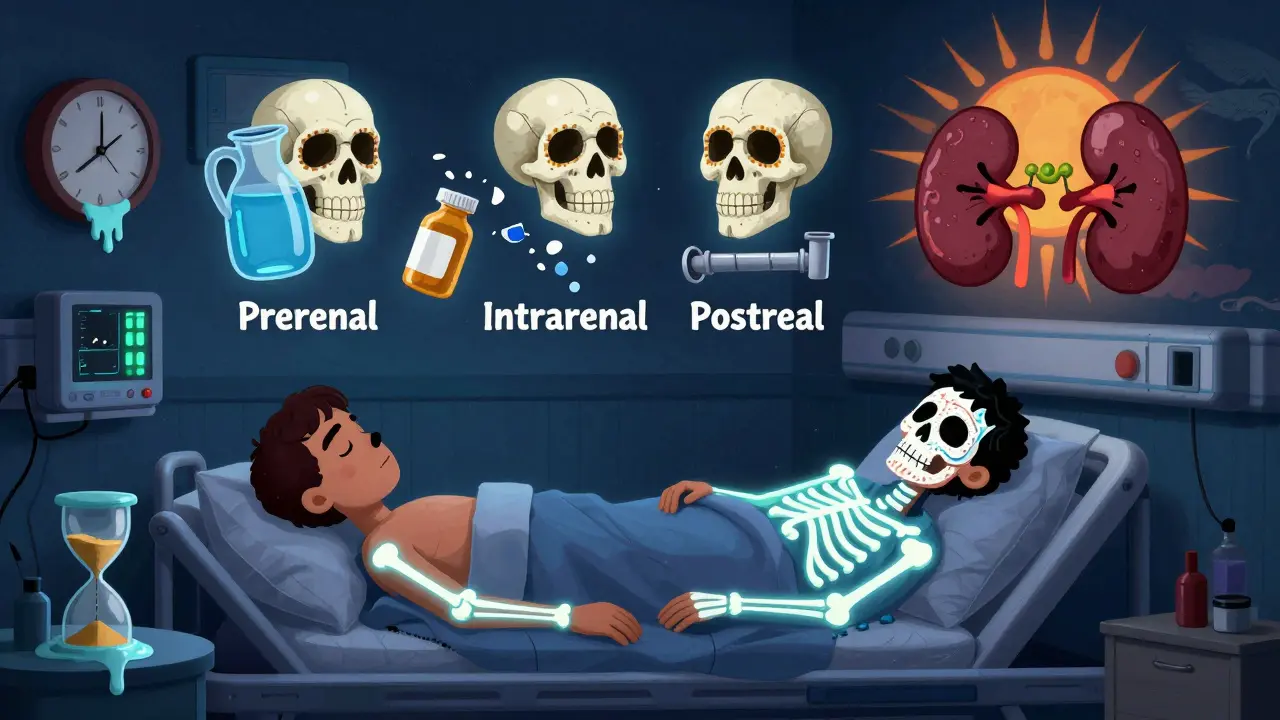
The Three Causes of AKI-and How They’re Treated
Not all AKI is the same. It’s broken into three types, each with a different fix.Prerenal AKI (60-70% of cases) means your kidneys aren’t getting enough blood. This isn’t a kidney problem-it’s a circulation problem. Dehydration from vomiting or not drinking enough? That’s it. Severe infection? Low blood pressure? Heart failure? All of these starve the kidneys. The fix? Fluids. Fast. A quick IV drip of saline can reverse this in 24 to 48 hours if caught early. No dialysis needed. No long-term damage. Just restore the flow.
Intrarenal AKI (25-35% of cases) means the kidney tissue itself is damaged. This is where things get serious. The most common cause? Acute Tubular Necrosis (ATN). Your kidney cells die from lack of oxygen or poison. What poison? Antibiotics like gentamicin. Contrast dye used in CT scans. Over-the-counter painkillers like ibuprofen if taken too long. Or a condition like glomerulonephritis, where your immune system attacks your kidneys. Treatment? Stop the toxin. Treat the infection. Use steroids for immune attacks. But recovery? It’s slower. Weeks, not days. Some people never fully bounce back.
Postrenal AKI (5-10% of cases) is a plumbing issue. Something blocks urine from leaving the kidney. In men over 60? Enlarged prostate. In anyone? Kidney stones. Cancer pressing on the ureters. If you don’t clear that blockage, pressure builds up and kills kidney tissue. The fix? A stent. A tube placed in the ureter to let urine flow again. Done right, kidney function often snaps back within hours.
How Doctors Diagnose It-And Why Timing Matters
There’s no single test for AKI. It’s a puzzle. First, they check your creatinine. A rise of 0.3 mg/dL in 48 hours? That’s AKI. A 50% jump in a week? Also AKI. Or if you’re peeing less than half a milliliter per kilogram of body weight for six hours-that’s the cutoff. But creatinine lags. It takes hours to rise after damage starts. That’s why doctors now watch urine output like a hawk in the ICU. Hourly measurements. No exceptions.Ultrasound is next. Is the kidney swollen? Are there stones? Is the bladder full? Ultrasound catches 85% of obstructions. If they suspect a blockage, a CT urogram finds stones with 95% accuracy. Blood tests look at BUN (blood urea nitrogen). High BUN with low sodium? That’s prerenal. High BUN with high sodium? Could be intrinsic damage. Fractional excretion of sodium (FeNa) tells them if the kidneys are trying to hold onto salt (prerenal) or if they’re already broken (intrinsic).
And now, new tools are emerging. Biomarkers like NGAL and TIMP-2/IGFBP7 can predict AKI 24 to 48 hours before creatinine rises. That’s huge. It means you might catch it before you even feel sick. Hospitals using these tests have cut AKI deaths by 12%. That’s not a small win.
Recovery Isn’t Guaranteed-And Who’s at Risk
Most people assume if you survive AKI, you’re fine. Not true. Only 70-80% of prerenal cases fully recover. For intrinsic AKI? Just 40-60%. If you had severe ATN and were oliguric for more than two weeks? Only 20-30% get back to normal. Age matters. If you’re over 65, your recovery chance drops by 35%. If your kidneys were already weak before-eGFR below 60? Recovery is half as likely. Need dialysis? Only 25% recover full kidney function by three months.And here’s the quiet crisis: 23% of AKI survivors develop chronic kidney disease within a year. Each episode of AKI raises your risk of needing dialysis five years later by more than eight times. That’s not a footnote. That’s a life-altering consequence.
But recovery isn’t just about numbers. One patient, after sepsis-induced AKI and 17 days on CRRT, said: “I was told my creatinine was normal. But I couldn’t walk 50 feet without collapsing. For three months, I felt like I was dragging a concrete block.” That’s kidney fatigue. It’s real. It’s long-lasting. And it’s rarely talked about.

What You Can Do-Before It Happens
AKI doesn’t always come out of nowhere. You can lower your risk.- Stay hydrated. Especially if you’re sick, on diuretics, or have heart or kidney disease.
- Avoid NSAIDs (ibuprofen, naproxen) if you’re dehydrated or have kidney disease. Even one dose can trigger AKI.
- Know your baseline creatinine. Ask your doctor for your last result. If it’s above 1.2 for men or 1.0 for women, you’re already at risk.
- Ask if contrast dye is truly necessary before a CT scan. Sometimes, an ultrasound or MRI can do the job without the risk.
- If you’re hospitalized, ask if they’re checking your urine output and creatinine daily. If they’re not, push for it.
There’s no magic pill. No supplement. No herbal remedy that prevents AKI. Just awareness. And action.
What Comes After Recovery
Even if your creatinine returns to normal, your kidneys aren’t done healing. Many need follow-up with a nephrologist within six months. Blood pressure control. Sugar control. No more NSAIDs. Regular kidney function tests. You might never need dialysis-but you’re now in a higher-risk group. That means monitoring, not ignoring.And mentally? The fear lingers. One survey found 42% of survivors had anxiety about their kidneys. That’s not paranoia. It’s trauma. You lived through a system failure. You saw your body break. You thought you might need lifelong dialysis. That doesn’t vanish when the numbers look good.
Recovery isn’t a finish line. It’s a new starting point.
Can acute kidney injury be reversed completely?
Yes, but it depends on the cause and how fast you get treatment. Prerenal AKI, caused by dehydration or low blood pressure, often reverses fully within days with fluids. Intrarenal AKI from drug damage or infection may take weeks, and some kidney cells are permanently lost. If you had severe ATN or needed dialysis, full recovery is less likely-only 25% regain normal function after dialysis. Early intervention is the biggest factor.
Is AKI the same as chronic kidney disease?
No. AKI is sudden and often reversible. Chronic kidney disease (CKD) is gradual, lasting three months or more, and usually permanent. But AKI can lead to CKD. About 23% of people who survive AKI develop stage 3 or higher CKD within a year. Each episode of AKI increases your long-term risk of kidney failure by more than eight times.
Can drinking more water prevent AKI?
It can help-especially if you’re at risk. Dehydration is the top cause of prerenal AKI. If you’re sick with vomiting or diarrhea, on diuretics, or have heart failure, staying hydrated lowers your risk. But drinking water won’t prevent AKI from drugs, infection, or blockages. It’s one tool, not a shield.
How long does it take to recover from AKI?
It varies. Prerenal AKI: 1-2 days with fluids. Intrarenal AKI: 2-6 weeks. Severe cases with prolonged low urine output: months, and sometimes not fully. Recovery isn’t just about creatinine levels-it’s about energy, stamina, and how your body feels. Many report fatigue for 3-6 months after recovery.
Do I need dialysis if I have AKI?
Not always. Only 5-10% of hospitalized AKI patients need dialysis. It’s reserved for life-threatening complications: high potassium, fluid overload, severe acidosis, or toxins building up. If you’re stable and the cause is treatable, dialysis isn’t needed. But if you do need it, your chances of full kidney recovery drop to 25%.
Can AKI happen to healthy people?
Yes. Even young, healthy people can get AKI. Dehydration from extreme exercise, a bad reaction to antibiotics, or a kidney stone can trigger it. One case involved a 28-year-old marathon runner who developed AKI after a 26-mile race without drinking enough. It’s not just for the elderly or sick.
AKI doesn’t care who you are. It doesn’t wait for permission. But with awareness, quick action, and proper care, many people walk away with their kidneys intact. The key? Don’t ignore the small signs. Your kidneys are working hard for you every minute. When they whisper, listen.







14 Comments
Brad Ralph February 11, 2026
So let me get this straight - your kidneys are basically the body’s water filter, and if you skip a few sips of water before a marathon, you’re one ibuprofen away from a hospital bed? 😅
Also, why is no one talking about how wild it is that we can now predict kidney failure before creatinine even spikes? That’s like having a smoke alarm for your organs.
Next thing you know, we’ll have AI that whispers to you at 3 a.m.: ‘Hey, you drank coffee after a night shift and didn’t pee in 8 hours. Maybe lay off the NSAIDs.’
Anyway. Just… hydrate. Please. I’m begging you.
Jim Johnson February 12, 2026
Man, I had a cousin go through this after a bad flu. Thought he was just ‘tired’ - turned out his creatinine was 4.8. They gave him fluids and he was walking in 3 days. But he still says he feels ‘heavy’ sometimes. Like his body’s still recovering from a ghost.
Don’t ignore the fatigue. Don’t brush off the nausea. And for god’s sake, if you’re on blood pressure meds or diuretics - stop popping Advil like M&M’s.
My mom’s a nurse. She says AKI is the silent killer because everyone thinks ‘kidney problems’ = old people. Nah. It’s runners. Nurses. People on antibiotics. Anyone.
Spread this. Please.
Pat Mun February 14, 2026
I work in a hospital unit and I see this every single week. People come in thinking they’re ‘just dehydrated’ - then we find their potassium is at 6.8. That’s not ‘a little off.’ That’s your heart about to tap out.
One guy? 42, triathlete, vegan, no meds. He took melatonin for sleep and ibuprofen for a headache after a 20-miler. Two days later - no urine. ICU. Dialysis for 11 days.
He’s fine now. But he can’t run again. And he says the worst part wasn’t the needles - it was the fear that he’d never feel ‘light’ again.
Don’t wait for symptoms. If you’re sick, dehydrated, or on meds - check your creatinine. Ask for a urine output log. If they say ‘we’ll check tomorrow’ - push back. Your kidneys don’t have a snooze button.
And yes - hydration helps. But it’s not magic. It’s just the first line of defense. Like wearing a seatbelt. Doesn’t guarantee safety - but it’s dumb not to.
Vamsi Krishna February 15, 2026
LOL so let me get this - you’re telling me that if I take a Tylenol after a party, my kidneys are gonna ‘shut down’? What’s next? Is my liver gonna start a protest? 😂
And why are we acting like this is new? My grandpa had AKI in 1978 from a UTI. He didn’t have NGAL biomarkers. He had a catheter and a prayer.
Also, why is this post so long? Did you copy-paste a textbook? I read 3 pages and my brain started crying.
Just say: Don’t take NSAIDs if you’re dehydrated. Don’t ignore no-pee. Drink water. Done.
Also - why is everyone so scared? Your kidneys are tough. They’ve survived your 20s. They’ll survive your 30s. Chill.
Alyssa Williams February 16, 2026
YES. This. I had AKI after a bad flu and dehydration. I thought I was ‘just tired.’ Turns out I was peeing 100ml a day. My doctor said if I’d waited 12 more hours, I’d have needed dialysis.
Now I carry a water bottle like it’s my soulmate. I check my urine color. I avoid ibuprofen. I ask for labs before CT scans.
And I tell everyone. Not to scare them - to empower them.
Your kidneys don’t scream. They whisper. And if you’re not listening? You’ll wake up in a hospital wondering why you didn’t drink more water.
Listen to your body. Not the ads. Not the ‘just take a pill’ culture. Your kidneys don’t have a mute button.
Carla McKinney February 18, 2026
It’s not ‘recovery’ - it’s survival. And let’s be real: the system doesn’t care. Hospitals don’t track long-term kidney fatigue. Insurance won’t pay for follow-ups. You’re just ‘stable’ now - so you’re fine.
Meanwhile, you’re still exhausted. Your legs feel like lead. You can’t sleep because your brain keeps replaying the ICU beeps.
This isn’t medicine. It’s a lottery. You get lucky? Great. You get unlucky? Welcome to lifelong monitoring, anxiety, and a 5x higher chance of dialysis in 5 years.
And guess who pays? You. Your family. Your future self.
So yeah. ‘Stay hydrated.’ Cute. But the real problem? We treat organs like disposable batteries.
Skilken Awe February 20, 2026
Let’s cut through the fluff. AKI isn’t ‘a medical emergency’ - it’s a failure of primary care. Why are we letting people get to ‘no urine’ before we check creatinine? Why aren’t we doing baseline labs on anyone over 40? Why is this even a ‘surprise’?
And don’t get me started on ‘biomarkers.’ You’re telling me we have a test that predicts AKI 48 hours early - but only 3 hospitals use it? Because ‘cost.’
So we’re prioritizing profit over function. Brilliant.
Also - ‘don’t take NSAIDs’? That’s like saying ‘don’t breathe air.’ Everyone takes ibuprofen. It’s in every medicine cabinet. You’re asking people to stop using a tool they’ve trusted for decades.
Don’t lecture. Fix the system.
Reggie McIntyre February 21, 2026
I’m a 34-year-old EMT. I’ve pulled over 20 people for AKI in the last year. One was 19 - came from a rave, didn’t drink water, took 4 Advil for ‘body aches.’
He didn’t even know what kidneys were. Said he thought they were ‘just for peeing.’
That’s the real tragedy. We’re not just treating organs - we’re trying to teach basic biology to people who’ve never been taught it.
And yeah - hydration helps. But the real fix? Education. In schools. In gyms. On social media. Not just in ERs.
My crew now carries pamphlets. We hand them out like candy. Because if you don’t know your body’s limits - you’ll break it.
christian jon February 22, 2026
Oh my GOD. I JUST HAD THIS HAPPEN TO MY BROTHER!!!
He took 2 Advil after a 10-mile run. Said he ‘felt fine.’ Next day? Swollen ankles. No pee. Called 911. They thought he was having a heart attack. Turned out his creatinine was 5.2. Dialysis for 8 days. Lost 15 pounds. Couldn’t walk. Still has ‘brain fog.’
He’s 31. Healthy. No history. Just thought ‘a little painkiller’ wouldn’t hurt.
Now he’s terrified of every headache. He won’t even take Tylenol without a doctor. His wife says he’s ‘a nervous wreck.’
THIS ISN’T A ‘MEDICAL CONDITION’ - IT’S A NATIONAL DISASTER. WHY ISN’T THE FDA DOING SOMETHING? WHY ISN’T PHARMACY CHAIN POSTING WARNINGS? WHY ISN’T EVERY DOCTOR SCREAMING THIS?
WE NEED A PUBLIC SERVICE CAMPAIGN. LIKE ‘DONT DRINK AND DRIVE.’ THIS IS ‘DONT TAKE NSAIDS IF YOU’RE DEHYDRATED.’
AND WHY DO WE STILL USE CREATININE AS THE GOLD STANDARD WHEN WE HAVE BETTER TOOLS? IT’S 2025. WE’RE STILL USING 1950S TECH?
THIS IS OUTRAGEOUS.
Neha Motiwala February 24, 2026
So let me get this - you’re saying if I drink water, I won’t get AKI? What about the people who drink 3 gallons a day and still get it? Or the ones who never take NSAIDs? Or the ones who had a CT scan with contrast and didn’t even know?
This post feels like fear-mongering. Like someone just made up a list of scary words and called it ‘science.’
Also - ‘23% develop CKD’? Where’s the source? Is that from a study? Or a blog?
I’ve had 3 relatives with ‘kidney issues.’ Two were fine. One died. So what’s the real risk? No one knows. We’re just scared.
Maybe the real problem? Overmedication. Overtesting. Overhysteria.
Just let people live. Don’t turn every headache into a death sentence.
andres az February 25, 2026
Why are we even talking about this? It’s 2025. We have AI. We have wearables. We have apps that track your hydration, sodium, and urine output.
So why are we still relying on doctors to ‘notice’ a 0.3 creatinine spike?
It’s not the patient’s fault. It’s the system. Hospitals don’t integrate data. Labs don’t alert. Pharmacies don’t warn.
And yet we blame the person who took ibuprofen?
This isn’t about awareness. It’s about infrastructure failure.
Also - ‘your kidneys whisper’? Cute. But if your phone can warn you about low battery, why can’t your body get a push notification?
Fix the tech. Not the people.
steve sunio February 25, 2026
AKI? More like A.K.I. - ‘Always Know I’m in trouble.’ 😂
Look - I’m from Nigeria. We don’t have dialysis machines in every village. People die because they can’t afford a creatinine test. So why are we here talking about biomarkers and NGAL?
First world problem. Drink water. Don’t take pills. Done.
But yeah - if you’re rich and have a smartwatch? Cool. You can monitor your kidneys like a Tesla battery.
For the rest of us? We just hope the fever breaks.
This post? Too much. Too fancy. Too American.
Autumn Frankart February 26, 2026
Let’s be real - this is all a cover-up.
Who benefits from AKI panic? Pharma. Hospitals. Labs. They make billions off dialysis. Off contrast dyes. Off ‘biomarker tests.’
And now they’re telling us to ‘avoid NSAIDs’ - but what if the real problem is that they’re pushing expensive alternatives?
Why isn’t anyone asking: Why are we letting corporations control kidney health?
And why is ‘hydration’ the only advice? What about clean water access? What about pollution? What about the fact that 30% of US tap water has trace pharmaceuticals?
They want you to blame yourself - so you don’t blame the system.
Drink water? Sure. But also - protest. Demand transparency. Stop trusting corporations with your kidneys.
Jim Johnson February 27, 2026
^This. My cousin’s doctor told him to ‘drink water’ - then billed him $1200 for a biomarker test the next day.
That’s not prevention. That’s profit.
But still - I’m glad I learned this. Even if the system’s broken, I’m not going to ignore my body anymore.
Hydrate. Check labs. Ask questions. Even if they roll their eyes.
It’s not perfect. But it’s better than waiting for the beep.