Every year, thousands of patients in the U.S. receive the wrong medication-not because of a bad drug, but because the wrong person got it. In pharmacies, where doses are dispensed by hand or machine, a single mix-up can lead to hospitalization, permanent harm, or even death. The fix isn’t complex: use two patient identifiers every single time. Yet, it’s still one of the most overlooked safety steps in healthcare.
Why Two Identifiers? It’s Not Just a Rule-It’s a Lifesaver
The requirement to use two patient identifiers isn’t some bureaucratic checkbox. It’s a direct response to real, preventable deaths. In 2003, The Joint Commission made it a National Patient Safety Goal (NPSG.01.01.01) after reviewing hundreds of cases where patients got the wrong drugs because staff only checked one piece of info-like a name on a wristband that didn’t match the chart. Here’s what counts as a valid identifier: full legal name, date of birth, medical record number, or phone number. What doesn’t? Room number. Floor number. Even “the guy in bed 3.” Those are locations, not identities. And locations change. People move. Records get mixed up. Relying on them is like trying to find your car in a parking lot by remembering which row it’s in-without knowing the make, model, or license plate. A 2020 study in JMIR Medical Informatics found that about 10% of serious drug interaction alerts in the U.S. go unnoticed because patient records are mismatched or duplicated. That’s roughly 6,000 people a year getting medications that could kill them because no one checked a second identifier.Manual Checks Alone Aren’t Enough
Many pharmacies still rely on pharmacists asking patients, “What’s your name and date of birth?” Then the pharmacist nods, checks the label, and hands over the bottle. Sounds simple. But it’s flawed. People forget their birthdates. They give nicknames. They’re in pain, confused, or speaking a different language. A 2024 Reddit thread from a community pharmacist described a woman who came in for her blood pressure med. She said her name was “Linda,” but the system showed “Lindsey.” The pharmacist assumed it was a typo and dispensed the prescription. Three days later, the patient called back: her real name was Lindsey. The wrong person had picked up her medication-and taken her antidepressant. Even when staff are careful, human error is inevitable. A 2020 review in BMJ Quality & Safety found no solid proof that having two people double-check prescriptions reduces errors. Why? Because if both people are looking at the same flawed info, they’ll both miss the mistake.Technology Changes the Game
The real breakthrough isn’t asking for two identifiers-it’s verifying them with technology. Barcode scanning at the point of dispensing has cut medication errors reaching patients by 75%, according to a 2012 study in the Journal of Patient Safety. Here’s how it works: the pharmacist scans the patient’s wristband (with name and MRN), then scans the medication. The system compares the two. If they don’t match, it stops everything. No guesswork. No assumptions. Even better: biometric systems. Imprivata’s palm-vein scanner, used in hospitals across the U.S., matches patients to their records with 94% accuracy. Compare that to hospitals without enterprise master patient index (EMPI) systems, where matches drop to just 17%. That gap isn’t a tech glitch-it’s a safety gap. EMPI systems act like a central database that links every patient record across departments, clinics, and hospitals. Without one, a patient might have three records: one under “John Smith,” another under “J. Smith,” and a third under “Jonathan Smith.” Each record has different allergies, medications, or lab results. When a pharmacist pulls up “John Smith,” they might see the wrong history. A biometric scan? It finds the right one-every time.
What Happens When You Skip the Second Identifier?
The consequences aren’t theoretical. In 2023, a patient was brought to an emergency room unconscious. The hospital created a new record because they couldn’t find him in the system. Days later, staff realized he’d been there before-under his middle name. His original record listed a deadly allergy to penicillin. He’d been given a penicillin-based antibiotic. He survived. But only because a nurse noticed the rash. That’s not rare. The Emergency Care Research Institute (ECRI) lists patient misidentification as one of the top 10 threats to patient safety. It causes wrong-medication errors, transfusion errors, wrong-site surgeries, and even babies being sent home with the wrong parents. Dr. James P. Bagian, a former VA patient safety director, put it bluntly: “The two-identifier rule is one of the most fundamental yet frequently violated safety protocols in healthcare.” And pharmacies? They’re ground zero.Real-World Challenges and How to Fix Them
You might think, “We do this already.” But compliance isn’t perfect. A 2023 survey by the American Society of Health-System Pharmacists found that 63% of pharmacists admitted to cutting corners during busy hours. In community pharmacies, 42% said they verify identifiers verbally-without writing it down. The Joint Commission found that in 37% of non-compliant hospitals, staff didn’t document the verification at all. That’s not just unsafe-it’s legally risky. If something goes wrong and there’s no record, the pharmacy can’t prove they followed protocol. Solutions exist:- Use timeouts before high-alert meds-like insulin or blood thinners. Stop. Scan. Confirm. Say it out loud.
- Implement EMPI to kill duplicate records. A 2023 KLAS Research report showed 68% of large health systems use EMPI. The ones that don’t spend an estimated $40 million a year fixing errors.
- Use biometrics where possible. A palm scan takes under 10 seconds. No memory needed. No mispronunciations. No fake names.
- Document every check. Not just “verified.” Write the identifiers used: “Name: Maria Gonzalez, DOB: 03/15/1972.”
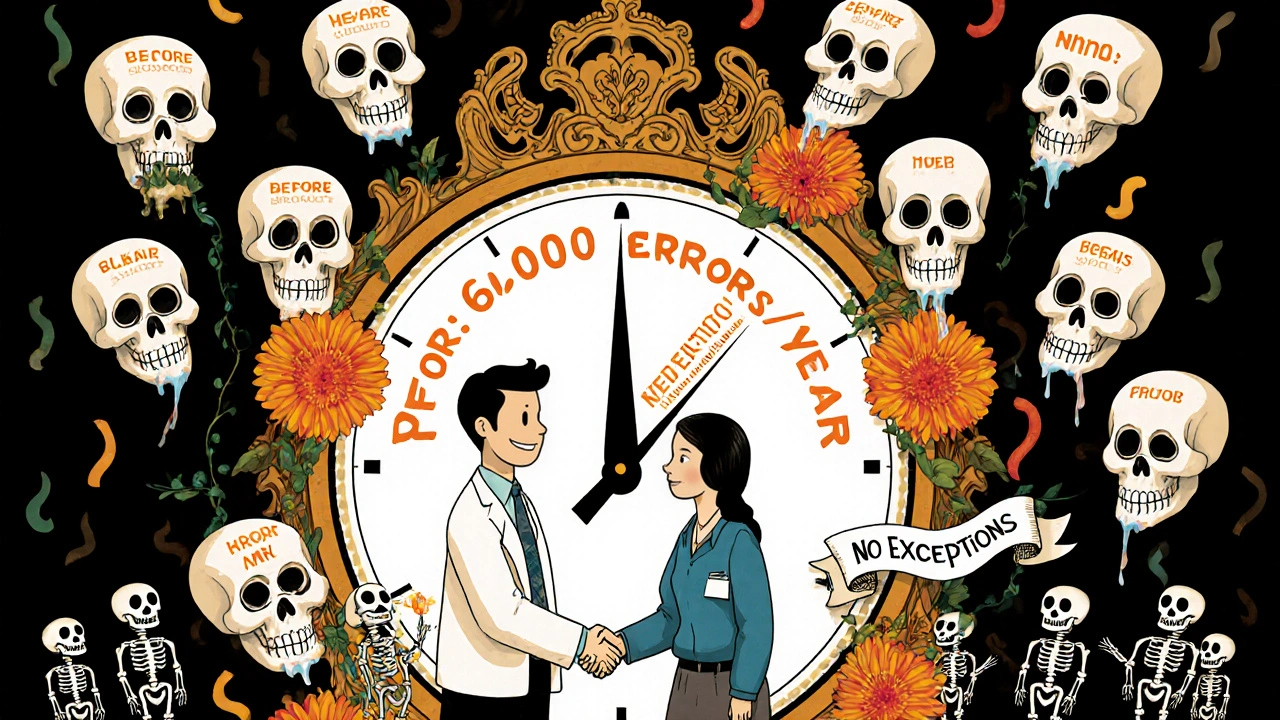
Regulations Are Getting Tougher
The Joint Commission doesn’t just recommend this-it enforces it. In 2023, non-compliance with the two-identifier rule was the third most common violation in hospital surveys. That’s not a minor slip. It’s a safety failure that can cost a hospital its accreditation. And without accreditation, Medicare and Medicaid payments stop. The 21st Century Cures Act and CMS rules now tie accurate patient identification to nationwide data sharing. If your records are messy, you can’t participate in health information exchanges. That means slower care, more delays, and more errors.The Future: A National Patient Identifier?
Right now, there’s no universal patient ID in the U.S. Like a Social Security number for health records. But that’s changing. In January 2025, a pilot program launched in five regional health exchanges to test a voluntary, opt-in national identifier system. The American Medical Informatics Association supports it. So do most patient safety experts. Why? Because a single identifier could cut duplicate records by 90%. It could make drug interaction alerts accurate. It could stop 6,000 people a year from getting the wrong meds. The barriers? Cost ($1.2-1.8 million per 100-bed hospital), legacy systems, and privacy fears. But the cost of inaction? Billions in wasted care, lawsuits, and lives lost.What You Can Do Today
Whether you’re a pharmacist, technician, or patient:- Always ask for two identifiers-never one. Even if the patient says, “I’m the only John Smith here.”
- Use technology if it’s available. Don’t trust memory. Trust the system.
- Document everything. If it’s not written, it didn’t happen.
- Speak up. If you see someone skipping the second check, say something. It’s not being a snitch-it’s saving a life.
Medication safety isn’t about having the smartest pharmacist or the fastest scanner. It’s about doing the simple thing, every time. Two identifiers. No exceptions. Because in pharmacy, the difference between life and death isn’t a complex algorithm-it’s a name and a birthdate.
What are the two acceptable patient identifiers in a pharmacy?
The Joint Commission requires at least two of the following: full legal name, date of birth, assigned medical record number, or telephone number. Room number, location, or gender are not acceptable because they aren’t unique to the individual.
Why can’t I just use the patient’s name and room number?
Room numbers change. Patients move. Two people can be in the same room. A name alone can be common-there are over 150,000 people named “John Smith” in the U.S. Using room number as an identifier is like using “the red car” to find a specific vehicle in a parking lot. It’s unreliable and dangerous.
Is verbal confirmation enough to verify patient identity?
No. Verbal confirmation without documentation is risky. The Joint Commission requires verification to be recorded in the patient’s medication administration record. A pharmacist saying, “I asked her name,” isn’t proof. Written or scanned records are the only defensible method.
How effective is barcode scanning compared to manual checks?
Barcode scanning reduces medication errors reaching patients by 75%, according to a 2012 study in the Journal of Patient Safety. Manual checks still have error rates of 1-3% per dose. Technology removes human assumptions and forces accurate matching.
What happens if a pharmacy doesn’t use two patient identifiers?
The pharmacy risks losing its accreditation from The Joint Commission. This can lead to loss of Medicare and Medicaid reimbursement. In the event of a medication error, the pharmacy can’t prove it followed safety protocols, exposing it to lawsuits and regulatory penalties.
Are there any exceptions to the two-identifier rule?
There are no exceptions for routine dispensing. Even for unconscious patients, staff must use the wristband barcode or EMPI system to identify them. In emergencies, if no identifier is available, the pharmacist must document the reason and consult with a prescriber before dispensing any medication.
How do duplicate medical records affect patient safety?
Duplicate records mean a patient’s allergy history, current meds, or lab results might be split across files. A pharmacist might see only one record and miss a life-threatening interaction. Studies show 8-12% of patient records in systems without EMPI are duplicated, contributing to an estimated $40 million in annual costs per large hospital.







12 Comments
Sharley Agarwal November 24, 2025
Two identifiers? Please. In India, we don’t even have IDs for half the population-how’s this supposed to work?
Erika Hunt November 25, 2025
I’ve worked in community pharmacy for 17 years, and I can tell you-this isn’t about technology, it’s about culture. We’ve got pharmacists who’ve been doing this since before barcode scanners existed, and they swear by their ‘system’-which is usually a glance, a nod, and a prayer. I’ve seen people hand out insulin to the wrong person because they ‘knew’ the guy in the blue jacket was Mr. Johnson. He wasn’t. He was just a guy with the same last name who came in for cough syrup. The system didn’t stop it. The patient’s daughter did-because she noticed her dad’s meds looked different. That’s the problem: we treat safety like a chore, not a sacred ritual. And no, saying ‘name and DOB’ out loud doesn’t count if you don’t write it down. The Joint Commission isn’t asking for perfection-they’re asking for documentation. And yet, 63% of pharmacists still cut corners. Why? Because no one’s watching. And when no one’s watching, human nature takes over. We get tired. We get busy. We assume. And assumptions kill. I’ve watched colleagues get reprimanded, lost licenses, even faced lawsuits-all because they thought ‘it’s just one time.’ But it’s never just one time. It’s always the next time. And the one after that. And the one after that. Until someone dies. And then, suddenly, everyone’s shocked. But we knew. We all knew. And we kept doing it anyway. Because it’s easier. And that’s the real tragedy here-not the lack of tech, but the lack of will.
Srikanth BH November 26, 2025
Hey, I get it-this stuff matters. But let’s not forget: in places where people don’t have birth certificates or medical records, this system breaks down. Maybe we need tech that adapts to people, not the other way around. A palm scan won’t help if someone’s never had a record to begin with. Let’s build bridges, not barriers.
Timothy Sadleir November 28, 2025
Let’s be honest: this whole two-identifier push is just another federal overreach disguised as safety. The real problem? The EMPI system is a data mine. Your name, DOB, MRN-all tied together in one central database? That’s a hacker’s dream. And don’t tell me it’s secure. The VA’s system was breached in 2017. Now they want to nationalize it? Please. We’re trading privacy for a 75% reduction in errors that could be solved with better training and common sense. And don’t even get me started on biometrics. Palm scans? Next they’ll be implanting chips. This isn’t healthcare reform-it’s surveillance capitalism with a stethoscope.
Kimberley Chronicle November 30, 2025
From a health informatics standpoint, the real bottleneck isn’t the two-identifier rule-it’s the lack of interoperability between EMPIs. Even with biometrics, if the master patient index isn’t harmonized across EHR platforms, you’re still dealing with fragmented data. The 94% accuracy rate cited? That’s only true in closed-loop systems. In the wild, where hospitals use Epic, Cerner, and Meditech, identity resolution drops to sub-50%. We need federated identity standards, not just better scanners. And yes-this is why the 21st Century Cures Act’s focus on FHIR and patient-matching APIs is so critical. Without standardized identifiers, we’re just rearranging deck chairs on the Titanic.
Jennifer Griffith December 2, 2025
lol why are we even talking about this? I work at a pharmacy and we just ask for name and last 4 of SSN. works fine. also, who even has a medical record number anymore? everyone’s on insurance now. this whole post feels like a 2010s hospital training video.
Roscoe Howard December 3, 2025
This is what happens when you let bureaucrats design safety protocols. In America, we used to rely on common sense and professional judgment. Now we need scanners, biometrics, and written logs just to hand someone a bottle of ibuprofen? This isn’t safety-it’s compliance theater. And don’t get me started on the cost. Every time a pharmacist has to stop and scan a wristband, they’re losing time. Time that could be spent counseling patients. We’re turning healthcare into a factory line, and the workers are the ones paying the price. And who benefits? The tech vendors. They’re laughing all the way to the bank while real pharmacists burn out.
prasad gaude December 4, 2025
Back home in Kerala, we used to identify patients by their mother’s name, their village, and the color of their shirt. It worked. Not because it was high-tech-but because it was human. In the West, we think technology fixes everything. But sometimes, the problem isn’t the system-it’s the distance we’ve created between people. A barcode doesn’t care if you’re scared. A palm scan won’t notice if your hands are shaking. Maybe the real solution isn’t more tech-but more presence. More listening. More remembering. Not just scanning.
Lisa Odence December 6, 2025
OMG I LOVE THIS POST!! 🙌 This is exactly why I quit my job at the ER last year-saw a baby get the wrong blood type because the nurse didn’t verify the second ID. I was crying in the break room. The system is broken. We need biometrics. We need EMPI. We need to stop trusting memory. And yes, I wrote down every single time I verified-name, DOB, MRN. Even if no one else did. I’m not just a pharmacist-I’m a guardian. And if you’re not documenting, you’re not caring. ❤️ #TwoIdentifiersNotOptional #PatientSafetyFirst
Patricia McElhinney December 6, 2025
Let me be clear: if your pharmacy doesn't use two identifiers, you are a criminal. Not negligent. Not careless. CRIMINAL. You are putting lives at risk for convenience. And if you think 'I've never had an error'-you're just lucky. Or you're lying. The Joint Commission isn't asking for a favor. They're enforcing the law. And if you can't follow basic safety rules, you shouldn't be handling controlled substances. Period. No exceptions. No excuses. No 'but I'm busy.' Your job isn't to be efficient-it's to be accurate. And if you can't handle that, go sell shoes.
Dolapo Eniola December 6, 2025
Y’all in the US think you’re so advanced with your scanners and EMPIs. In Nigeria, we don’t even have national IDs for 40% of people. But we still don’t kill people with wrong meds. Why? Because we talk to them. We know their family. We know their face. We don’t need a barcode to know who’s who. Your tech is a crutch. Your bureaucracy is a mask. Real safety isn’t in systems-it’s in relationships. And you’ve forgotten that.
Shirou Spade December 7, 2025
There’s a deeper truth here: we’ve outsourced trust to machines. We used to believe in the pharmacist’s word. Now we believe in the beep of a scanner. But what happens when the machine fails? What happens when the barcode doesn’t scan? What happens when the palm scan can’t read a calloused hand? We’ve built a system that punishes the imperfect-people with faded tattoos, elderly hands, immigrants without proper IDs-and we call it progress. But progress without compassion is just automation. And automation without humanity? That’s not safety. That’s silence.