DVT Risk Factor Assessment Tool
Your Risk Assessment
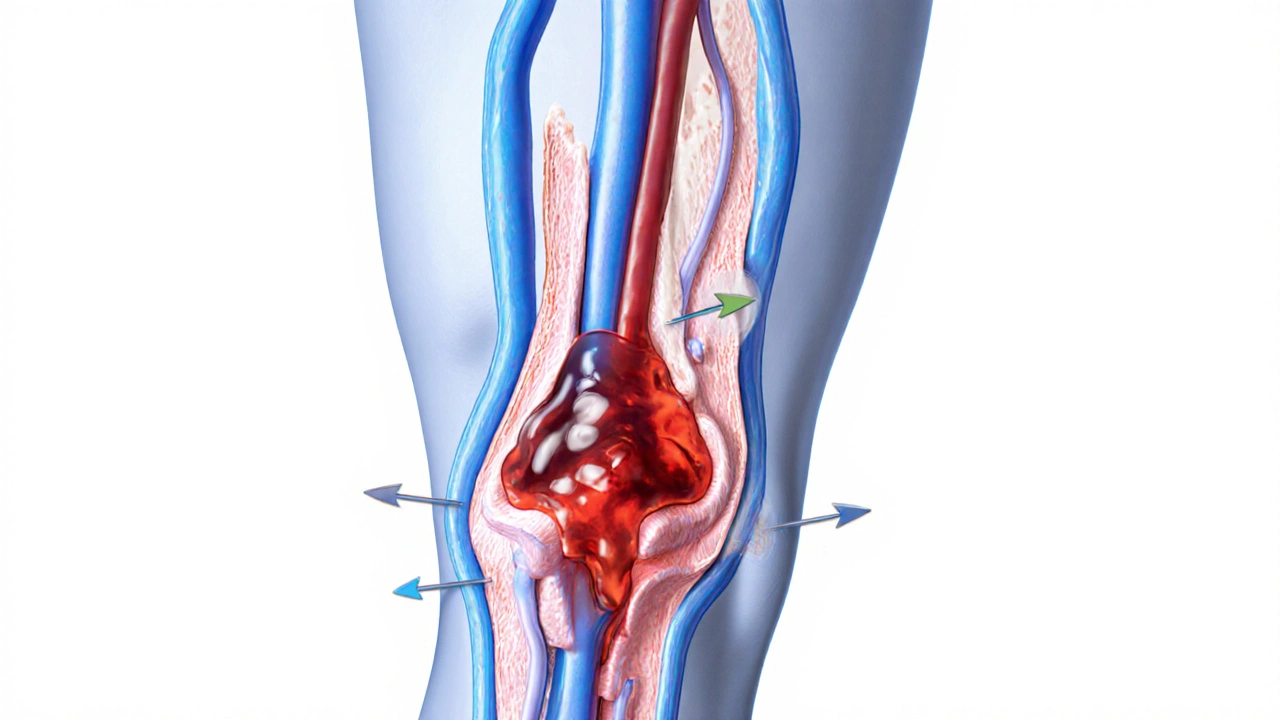
When a blood clot forms inside a deep vein-usually in the leg-it’s called Deep Vein Thrombosis is a dangerous condition where a clot blocks venous flow, potentially leading to swelling, pain, and, if it travels to the lungs, a pulmonary embolism. Knowing why it happens and how to stop it can save lives, especially for people with hidden risk factors.
What Is a Blood Clot and How Does DVT Develop?
A blood clot is a gelatinous mass of platelets and fibrin that forms to seal a wound. In a healthy system, clots appear only when needed and dissolve quickly. Deep veins, however, have slower blood flow, making them prime spots for clots to linger. When a clot grows, it narrows the vein, causing pain, redness, and swelling-classic DVT symptoms.
Key Risk Factors Behind DVT
Doctors often point to three pillars that create a perfect storm for clot formation: venous stasis, hypercoagulability, and endothelial injury. Below is a quick rundown of the most common contributors.
- Venous stasis: prolonged immobility (long flights, bed rest after surgery) slows blood return to the heart.
- Hypercoagulability: genetic traits like Factor V Leiden a mutation that makes blood clot more readily, cancer, or hormonal therapy raise clotting tendency.
- Endothelial injury: trauma to the vein wall from surgery, IV catheters, or severe inflammation.
- Age over 60, obesity, and smoking further tip the balance.
Understanding which of these you’re exposed to helps you target prevention.
Quick Takeaways
- DVT occurs when a clot blocks a deep vein, most often in the leg.
- Three main risk pillars: venous stasis, hypercoagulability, endothelial injury.
- Short‑term immobility is a fast‑acting trigger; long‑term factors include genetics and chronic disease.
- Prevention blends movement, compression, and medication when needed.
- Early symptom recognition (pain, swelling, warm skin) speeds treatment and cuts complications.
Prevention Strategies You Can Start Today
Prevention isn’t a one‑size‑fits‑all plan. It combines lifestyle tweaks, mechanical aids, and, for high‑risk folks, medication.
1. Keep Blood Flow Moving
Simple habits can offset venous stasis:
- Stand up and walk for a few minutes every hour during long trips or desk work.
- Do ankle pumps-flex and point your toes-to activate calf muscles.
- Stay hydrated; dehydration thickens blood.
2. Compression Stockings
Compression stockings are specially fitted garments that apply graduated pressure to the lower leg, encouraging venous return are proven to lower DVT rates after surgery. Choose the right compression level (15‑20mmHg for moderate risk, 20‑30mmHg for higher risk) and wear them as directed.
3. Anticoagulant Therapy
When a person’s clotting risk is high, doctors prescribe blood thinners. Two main families dominate:
- Warfarin a vitamin K antagonist that requires regular INR monitoring.
- Direct oral anticoagulants (DOACs) like apixaban and rivaroxaban-no routine blood tests needed, quicker onset.
Medication choice hinges on kidney function, drug interactions, and patient preference.
Comparing Medication vs. Mechanical Prevention
| Method | Typical Use Cases | Advantages | Disadvantages |
|---|---|---|---|
| Anticoagulant Therapy | Post‑operative patients, cancer, inherited clotting disorders | Highly effective at preventing clot extension; reduces mortality | Bleeding risk; requires monitoring (warfarin) or cost considerations (DOACs) |
| Compression Stockings | Orthopedic surgery, long‑haul travel, moderate‑risk outpatients | Non‑invasive; minimal side‑effects; easy to use | Discomfort if ill‑fitted; less effective for very high‑risk patients |
| Intermittent Pneumatic Compression (IPC) | Major abdominal or pelvic surgery, trauma patients | Mechanical mimic of muscle pump; works when patients can’t move | Requires device; can be costly; patient compliance needed |
When to Seek Medical Attention
If you notice sudden leg swelling, a warm or red area, or pain that feels like cramping, call a doctor immediately. These signs often point to DVT, and early treatment can prevent a pulmonary embolism.

Managing DVT After Diagnosis
Once diagnosed, treatment follows three steps:
- Stabilize: Start anticoagulant (usually a DOAC) within hours.
- Prevent Recurrence: Continue medication for 3‑6 months (or longer if risk persists).
- Rehab: Use compression stockings and gentle calf exercises to restore circulation.
Regular follow‑ups ensure the clot dissolves and the vein heals.
Common Pitfalls and How to Avoid Them
- Skipping early movement: Even short walks after surgery dramatically cut DVT rates.
- Using the wrong compression level: Too low offers no protection; too high can cause skin damage.
- Ignoring medication side‑effects: Report unusual bruising or bleeding to your doctor right away.
- Assuming low risk: Family history of clotting disorders raises risk, even for young, active people.
FAQs
What are the earliest signs of Deep Vein Thrombosis?
Swelling, pain that feels like a cramp, warmth, and a reddish hue on the affected leg are the most common early warnings. If any of these appear after a period of immobility, seek care right away.
Can I prevent DVT without medication?
Yes. Regular movement, proper hydration, and wearing correctly fitted compression stockings are effective for low‑to‑moderate risk individuals. Mechanical devices like IPC can also help when movement is limited.
How long should I wear compression stockings after surgery?
Most surgeons advise wearing them continuously for 10‑14 days, then during waking hours for up to 6 weeks, depending on the type of surgery and personal risk profile.
Are DOACs safer than warfarin?
Direct oral anticoagulants have a lower risk of major bleeding and don’t require routine INR monitoring, making them a convenient choice for many patients. However, warfarin is still preferred for people with certain kidney issues or mechanical heart valves.
If I have a genetic clotting disorder, can I still travel safely?
Travel is possible, but you should discuss prophylactic measures with your doctor-often a low‑dose anticoagulant or compression stockings during the flight-and avoid long periods of immobility.






11 Comments
Murhari Patil October 8, 2025
They don’t tell you that the hospitals are hiding a secret: every surgery is a DVT trap, lurking in the shadows of sterile gowns.
kevin joyce October 9, 2025
When we contemplate the cascade of coagulation factors, we realize that stasis is not merely a passive state but an active invitation to pathology. The interplay of endothelial injury and hypercoagulability can be seen as a tragic drama of the circulatory system, urging us to intervene with both mechanical and pharmacologic strategies.
michael henrique October 9, 2025
Our nation’s health policy must enforce mandatory DVT prophylaxis for any patient immobilized longer than three days. No excuse, no delay, and no compromise on compression therapy or anticoagulation when indicated.
Nondumiso Sotsaka October 10, 2025
Keep moving, even a short walk can melt away the danger of clot formation 😊 Remember to hydrate and stretch those calves regularly!
Ashley Allen October 10, 2025
Compression stockings work.
Brufsky Oxford October 10, 2025
Indeed, the vascular rhythm mirrors the heart of existence 😊
Lisa Friedman October 11, 2025
It’s obvious that most peopel noot understand that DVT isn’t just a “old person” issue. The data shows even young athletes can get clots if they ignor proper hydration and movement. Trust me i’ve read the studies.
cris wasala October 11, 2025
Every step you take is a win against DVT keep it up you’ve got this
Tyler Johnson October 12, 2025
Understanding DVT requires us to look at the three pillars of Virchow: stasis, hypercoagulability, and endothelial injury, each contributing in its own subtle way. When a person sits for hours on a cramped flight, venous return slows, creating a perfect environment for platelets to aggregate. Similarly, after surgery, trauma to the vein wall releases tissue factor, kick‑starting the clotting cascade. Genetic predispositions such as Factor V Leiden add a hidden layer of risk that many are unaware of until a clot forms. Obesity and smoking further tip the balance, turning a marginal situation into a serious threat. Hydration is often overlooked, yet water thins the blood, facilitating smoother flow through the veins. Simple ankle pumps, like pointing and flexing the toes, activate the calf muscle pump and can dramatically cut stasis. Compression stockings, when properly fitted, apply graduated pressure that mimics natural muscle action, keeping blood moving upward toward the heart. For those at high risk, anticoagulant therapy such as DOACs provides a pharmacologic safeguard, though it comes with its own bleeding concerns. The decision between medication and mechanical prophylaxis should be individualized, weighing factors like kidney function and patient preference. Early recognition of symptoms – swelling, warmth, and a cramp‑like pain – can lead to prompt imaging and treatment, preventing pulmonary embolism. Follow‑up care, including continued use of compression garments and gradual re‑introduction of activity, ensures the vein heals properly. Education is key: patients must understand why they’re asked to move every hour and how to perform simple calf exercises. Healthcare providers should reinforce these messages at discharge, providing written instructions and possibly reminder tools. Ultimately, a combination of movement, proper compression, and, when needed, medication offers the best defense against this silent killer.
Annie Thompson October 12, 2025
Reading that thorough explanation made me feel both hopeful and terrified at the same time because the reality of clot formation is so close to our daily routines it feels like an invisible monster lurking in every chair we sit in and every long car ride we take I wish we could all just remember to stand up and stretch but life gets busy and sometimes we forget the simple act of moving our legs can be a lifesaver this article really opened my eyes and now I’m determined to set reminders on my phone and maybe even buy those compression stockings that look so comfy and protective
Parth Gohil October 12, 2025
From a practical standpoint, the take‑home is simple: keep the blood flowing, stay hydrated, and use compression gear when you know you’ll be immobile for a while – it’s a low‑effort, high‑reward strategy that fits nicely into any routine.