Why generic prescribing isn't just about saving money
You walk into a clinic, and your doctor hands you a prescription. You see the name on the bottle: atorvastatin. You expected Lipitor. You pause. Is this the same thing? Will it work? You’re not alone. Millions of patients have this moment. But here’s the truth: generic prescribing isn’t a cost-cutting trick. It’s the standard of care - backed by science, regulation, and decades of real-world use.
When a doctor writes a prescription for atorvastatin instead of Lipitor, they’re not cutting corners. They’re following guidelines from the NHS, the FDA, and the American College of Physicians. These guidelines say: prescribe by the active ingredient - the International Non-proprietary Name (INN). That’s it. And for 90% of medications, that’s all you need.
How generic drugs are proven to be the same
Generic drugs aren’t knockoffs. They’re not cheaper because they’re weaker. They’re cheaper because the patent expired, and other companies can make the same molecule without spending millions on research.
The FDA requires every generic drug to meet strict standards. It must have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. That’s not opinion - it’s law under the Hatch-Waxman Act of 1984. But the real test? Bioequivalence.
Before a generic can be approved, it must show it releases the same amount of drug into the bloodstream at the same rate as the brand. The acceptable range? 80% to 125% of the brand’s levels. That’s not a wide gap - it’s tighter than the variation you’d see if you took the same brand-name pill twice on different days.
The European Medicines Agency (EMA) and the World Health Organization’s INN program enforce the same rules. Over 190 countries use these standards. If a generic drug is on the market, it’s been tested to work like the brand. Not “kind of.” Not “mostly.” Exactly.
When you should still prescribe the brand name
Generic prescribing is the default - but not the only option. There are real exceptions. And ignoring them can harm patients.
The British National Formulary (BNF) identifies three clear categories where brand-name prescribing is still recommended:
- Narrow therapeutic index drugs - where small changes in blood levels can cause serious effects. Think: warfarin, levothyroxine, phenytoin, carbamazepine, and digoxin. Even a 10% difference in absorption can lead to under-treatment or toxicity.
- Modified-release formulations - like extended-release theophylline or certain ADHD medications. The way the drug is released over time matters. Not all generics replicate this perfectly.
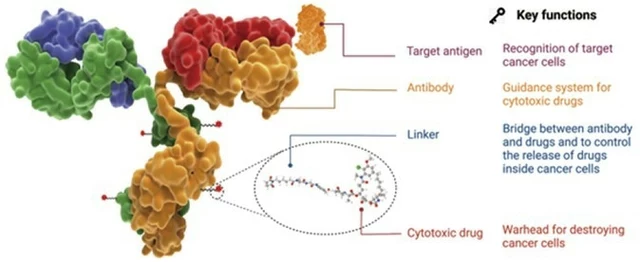
- Biologics and biosimilars - drugs made from living cells, like Humira or Enbrel. These are complex. The MHRA and FDA require brand-name prescribing here because switching between biosimilars and originators can trigger immune reactions.
That’s about 2% of all prescriptions. But those 2% matter. If you’re managing a patient on warfarin, you don’t switch brands unless you’re monitoring INR levels closely. If they’re on levothyroxine and suddenly feel fatigued after a switch, check their TSH. It’s not paranoia - it’s protocol.

Why patients resist - and how to fix it
Here’s the uncomfortable truth: patients often think generics are inferior. It’s not because they’re wrong. It’s because they’ve been told - by ads, by rumors, by old habits - that “brand” means better.
A 2021 study of 3,200 patients found that when doctors simply explained the science behind generics, patient acceptance jumped from 67% to 89%. That’s not magic. That’s communication.
Use this script: “This generic version has the same active ingredient as the brand you’ve been taking. It’s been tested to work the same way. The only difference is the price - it’ll save you about $15 a month, with no change in how it works.”
Don’t say: “It’s cheaper.” Say: “It’s the same medicine.”
And listen. If a patient says, “I felt different after switching,” don’t dismiss it. Check adherence. Check lab values. Check for the nocebo effect - where expecting a problem causes real symptoms. Studies show up to 30% of reported side effects from generic switches are psychological, not biological.
The real impact: cost, safety, and adherence
Let’s talk numbers. In the UK, switching to generic prescribing saves the NHS £1.3 billion a year. In the US, generic drugs saved $313 billion in 2019 alone. That’s not a drop in the bucket. That’s enough to fund thousands of primary care visits.
But the benefits go beyond money.
Patients who pay less for meds are more likely to take them. A JAMA study found generic prescribing improves adherence by 8-12%. That means fewer hospitalizations for heart failure, fewer ER visits for uncontrolled diabetes, fewer readmissions for depression.
And here’s a surprising benefit: fewer medication errors. When you prescribe “atorvastatin,” not “Lipitor,” “Atorva,” “Atorvastatin Teva,” or “Atorvastatin Mylan,” you cut down on confusion. The Institute for Safe Medication Practices found generic prescribing reduces errors by 50% - because there’s only one name to remember.
What’s changing in 2025
Generic prescribing isn’t static. It’s evolving.
In 2023, the FDA updated its rules under GDUFA III, requiring manufacturers to report adverse events tied to formulation differences. That means better tracking of subtle issues - like a generic that’s slightly slower to dissolve in some patients.
NHS England is pushing for 92% generic prescribing by March 2024. Electronic prescribing systems now default to generic names. Prescribers have to actively choose the brand - not the other way around.
And complex generics? Like inhalers or topical creams? Those are getting harder to copy. In 2022, 22% of applications for these were rejected because manufacturers couldn’t prove they matched the brand’s performance. That’s a good thing. It means regulators aren’t cutting corners.
The future isn’t just “more generics.” It’s smarter substitution. Using real-world data to decide who can switch safely - and who needs brand continuity. For most, it’s fine. For a few, it’s critical to hold the line.
What you need to do right now
You don’t need to memorize 50 drugs. You need to know the framework.
- Default to generic. Write the INN. Every time.
- Know the exceptions. Warfarin, levothyroxine, phenytoin, carbamazepine, digoxin, modified-release theophylline, biologics - these are your red flags.
- Explain it simply. Patients don’t need pharmacokinetics. They need to know: “This is the same drug. It’s cheaper. It works the same.”
- Monitor the high-risk. If you switch someone on warfarin or levothyroxine, check labs within 4-6 weeks.
- Use your system. Most EHRs now flag high-risk drugs. Let them help you.
Generic prescribing isn’t about forcing patients to accept less. It’s about giving them the same medicine at a fair price - without the hype. And when you do it right, you’re not just saving money. You’re saving lives.
Are generic drugs as effective as brand-name drugs?
Yes - for the vast majority of medications. Generic drugs must meet the same strict standards as brand-name drugs for active ingredients, strength, dosage form, and bioequivalence. The FDA and EMA require generics to deliver the same amount of drug into the bloodstream at the same rate as the brand, within a 80-125% range. Studies show no difference in clinical outcomes for over 98% of generic prescriptions.
When should I avoid prescribing a generic drug?
Avoid switching when the drug has a narrow therapeutic index - like warfarin, levothyroxine, phenytoin, carbamazepine, or digoxin - because small changes in blood levels can cause serious side effects. Also avoid switching for modified-release formulations (e.g., extended-release theophylline) and all biologic drugs (e.g., Humira, Enbrel). For these, brand-name prescribing is recommended to ensure consistent dosing and avoid immune reactions or loss of control.
Why do some patients say generics don’t work for them?
In most cases, it’s not the drug - it’s the expectation. Studies show up to 30% of reported side effects or reduced effectiveness after switching to generics are due to the nocebo effect - where patients believe generics are inferior, so they feel worse. But some patients do have real issues, especially with complex drugs like thyroid meds or antiepileptics. Always listen, check labs, and don’t assume it’s “all in their head.”
Do generics have different side effects?
The active ingredient - the part that treats your condition - is identical. Side effects from that ingredient will be the same. But inactive ingredients (fillers, dyes, coatings) can differ. These rarely cause problems, but in rare cases, they may trigger allergies or affect absorption in sensitive patients. If a patient reports new side effects after switching, investigate the cause - it’s not always the generic.
Can pharmacists substitute generics without my approval?
In most places, yes - unless you write “Dispense as Written” or “Do Not Substitute” on the prescription. But you can control this. Write the generic name (INN) to allow substitution. Write the brand name only if it’s clinically necessary (e.g., for narrow therapeutic index drugs or biologics). Your prescription language tells the pharmacist what to do.
Is there a difference between generic manufacturers?
All approved generics must meet the same standards. But for complex drugs - like modified-release tablets or inhalers - minor formulation differences can affect how the drug is absorbed. That’s why the FDA and NHS track these closely. If a patient does well on one generic, stick with it. Don’t switch between manufacturers unless necessary. Consistency matters more than the brand name.
What’s next for generic prescribing?
The goal isn’t to eliminate brand-name drugs. It’s to use them wisely.
For 98% of prescriptions, the generic is the right choice - safer, cheaper, and just as effective. For the other 2%, the brand is necessary. The job of the prescriber isn’t to pick one over the other blindly. It’s to know when each one belongs.
As technology improves - with AI tools flagging high-risk switches and real-world data guiding personalized decisions - we’ll get even better at matching the right drug to the right patient.
But the core hasn’t changed. If a drug works as a generic, prescribe it. If it doesn’t, prescribe the brand. And always, always explain why.





15 Comments
Liam Strachan November 20, 2025
Been prescribing generics for years now and honestly? Patients barely notice the difference. The real win is when they actually fill the script instead of letting it sit in their wallet. Saved my clinic a ton of headaches.
Gerald Cheruiyot November 21, 2025
Generics aren't just cheaper-they're the logical endpoint of medicine evolving beyond corporate branding. We're not selling soap. We're healing people. The molecule doesn't care what label it's on.
Michael Fessler November 22, 2025
bioequivalence is key but let's be real-some generics have different excipients that can affect GI absorption, especially in patients with IBS or malabsorption syndromes. not always the nocebo effect. i've seen patients crash on levothyroxine switches because the filler changed the dissolution profile. check labs. always.
daniel lopez November 22, 2025
they're lying to you. the FDA lets generics in that are 20% weaker and 25% stronger. that's not science-that's corporate corruption. Big Pharma owns the regulators. You think they want you saving money? They want you hooked on $300 pills. Wake up.
Ron and Gill Day November 24, 2025
This is the most condescending, oversimplified piece of medical propaganda I've read all year. You act like patients are idiots who need to be spoon-fed 'it's the same medicine.' The reality is complex. You're not saving lives-you're enabling cost-cutting at the expense of clinical nuance.
Alyssa Torres November 24, 2025
I had a patient cry because she switched from Lipitor to atorvastatin and felt 'empty'-like her body didn't recognize it. We checked labs-same numbers. But she felt better when we switched back. Turns out, the ritual of taking the blue pill mattered to her. Medicine isn't just chemistry. It's trust.
Summer Joy November 25, 2025
Oh wow, another 'trust the science' lecture. 🙄 Meanwhile, my cousin had a seizure after switching generics for carbamazepine. No one listened. Now she's on disability. Thanks for your 'framework,' Dr. Smug.
Aruna Urban Planner November 25, 2025
In India, generics are the only option for most. But we have a problem: quality control varies wildly between manufacturers. The FDA standards are gold. Many Indian generics don't meet them. So when we say 'it's the same,' we need to specify which generic. Not all are created equal.
Nicole Ziegler November 27, 2025
my grandma takes her generics and says they work fine. she also says her phone is too slow. both are true. 🤷♀️
Bharat Alasandi November 27, 2025
bro in rural india we dont even have brand names. its just 'blood pressure pill' or 'diabetes pill'. if it works, its good. if it dont, we find another. simple. no drama. no marketing. just medicine.
Kristi Bennardo November 28, 2025
This article is dangerously naive. You are normalizing pharmaceutical negligence under the guise of cost-efficiency. When a patient suffers due to an unapproved generic substitution, who takes responsibility? Not you. Not the pharmacist. Just another statistic.
Shiv Karan Singh November 30, 2025
everyone says generics are fine until their kid needs epilepsy meds. then suddenly it's 'oh no the filler changed!' hypocrites. you want cheap? fine. but don't act like you care about safety when you're just mad you can't get your brand-name Xanax anymore.
Ravi boy November 30, 2025
in india we call generics 'copy pills' and they work fine. if you have money buy brand if not copy is fine. no need for lectures. also typo sorry
Matthew Karrs December 2, 2025
the 2% exceptions? That's 100 million prescriptions in the US alone. You're treating a systemic risk like it's a footnote. And don't get me started on how pharmacists substitute without telling the patient. This isn't progress-it's a liability waiting to explode.
Matthew Peters December 4, 2025
my dad switched to generic warfarin and his INR went from 2.4 to 4.8 in two weeks. no warning. no lab check. just 'it's the same.' he almost bled out. now he only takes the brand. and yeah, it's expensive. but he's alive. so I'm good with that.