When your heart muscle stops working the way it should, it doesn’t just feel like fatigue-it can be life-threatening. Cardiomyopathy isn’t one disease. It’s a group of conditions that attack the heart muscle directly, making it harder to pump blood. And while many people think of heart disease as clogged arteries, cardiomyopathy is different. It’s about the muscle itself-thickened, stretched, or stiffened-without being caused by high blood pressure or blocked arteries. The three main types-dilated, hypertrophic, and restrictive-each behave in unique ways, require different tests, and demand completely different treatments.
Dilated Cardiomyopathy: The Heart That’s Too Big and Too Weak
Dilated cardiomyopathy (DCM) is the most common type, making up about half of all cases. Imagine your heart’s main pumping chamber-the left ventricle-stretching out like an old balloon. It gets bigger, thinner, and weaker. Instead of squeezing hard to push blood out, it just flops. That’s DCM. The ejection fraction-a measure of how much blood the heart pumps with each beat-drops below 40%. Normal is 55% to 70%.
People with DCM often feel winded climbing stairs, swollen in the legs, or like they can’t catch their breath lying down. Some don’t notice symptoms until they’re in heart failure. The causes? They vary. About one in three cases are genetic, passed down through families via mutations in genes like TTN or LMNA. Others come from long-term alcohol abuse-more than 80 grams a day for five years can damage the heart muscle. Viral infections, like coxsackievirus, can trigger it. Chemotherapy drugs like doxorubicin are another known culprit, especially after cumulative doses over 450 mg/m².
Diagnosis starts with an echocardiogram. If the left ventricle is larger than 55 mm in men or 50 mm in women, and the wall is thin (under 10 mm), DCM is likely. Cardiac MRI confirms it by spotting scar tissue or fibrosis in the muscle. Genetic testing is recommended if there’s a family history-about 25% to 35% of DCM cases are inherited.
Treatment isn’t about fixing the shape. It’s about supporting the weak pump. Guideline-directed medical therapy (GDMT) includes ARNIs like sacubitril/valsartan, beta-blockers, SGLT2 inhibitors, and sometimes aldosterone blockers. These drugs don’t cure it, but they cut death risk by 30% over three years. In severe cases, an ICD (implantable cardioverter-defibrillator) may be implanted to prevent sudden cardiac arrest. For the 10% who don’t respond, a heart transplant may be the only option.
Hypertrophic Cardiomyopathy: The Heart That’s Too Thick
Hypertrophic cardiomyopathy (HCM) is the opposite problem: the heart muscle gets unnaturally thick, especially in the septum-the wall between the two lower chambers. This isn’t from exercise or high blood pressure. It’s genetic. About 60% of cases involve mutations in sarcomere genes like MYH7 or MYBPC3. It’s inherited in an autosomal dominant pattern, meaning if one parent has it, each child has a 50% chance of getting it.
HCM affects roughly 1 in 500 people, but many go undiagnosed-especially athletes. In fact, it’s the leading cause of sudden cardiac death in young athletes under 35. The thickened muscle doesn’t just make the heart stiff-it can block blood flow out of the ventricle. This is called obstructive HCM, and it happens in about 70% of cases. When that happens, the pressure gradient across the outflow tract hits 30 mmHg or more, causing dizziness, chest pain, or fainting during activity.
Diagnosis relies on echocardiography. A wall thickness of 15 mm or more (or 13 mm if a relative has HCM) confirms it. Cardiac MRI shows the exact pattern of thickening and can detect fibrosis. Genetic testing identifies the mutation in about 60% of cases. But here’s the catch: having the gene doesn’t mean you’ll have symptoms. That’s why family screening is critical.
Treatment focuses on reducing symptoms and preventing sudden death. Beta-blockers like metoprolol help relax the heart and slow the pulse, improving symptoms in 70% of patients. For those with obstruction, disopyramide (a heart rhythm drug) can help. But for severe cases, doctors may perform septal reduction therapy-either surgically removing part of the thickened muscle or using alcohol to destroy it. About 85% of patients report immediate relief. An ICD is recommended for those with high-risk features: family history of sudden death, unexplained fainting, or abnormal blood pressure during exercise.
In 2022, the FDA approved mavacamten (Camzyos), the first drug specifically designed for obstructive HCM. It reduces the muscle’s hypercontractility, lowering outflow gradients by 80% in clinical trials. But it costs $145,000 a year-and requires strict monitoring because it can lower the heart’s pumping ability too much.
Restrictive Cardiomyopathy: The Heart That Won’t Fill
Restrictive cardiomyopathy (RCM) is the rarest, making up only 5% of cases. Unlike DCM or HCM, the heart muscle doesn’t stretch or thicken-it just gets stiff. Think of it like a heart wrapped in rubber. It can still squeeze fine, but it can’t relax enough to fill with blood. So even though the pumping action looks normal (ejection fraction stays above 50%), the heart doesn’t get enough blood in between beats.
RCM isn’t usually inherited. It’s caused by other diseases that infiltrate the heart. Amyloidosis is the biggest culprit-60% of cases. This is when abnormal proteins build up in the heart tissue. Sarcoidosis, hemochromatosis (too much iron), and Fabry disease are other causes. These conditions don’t just affect the heart; they damage other organs too.
Diagnosis is tricky. Echocardiography shows a small, stiff ventricle with a classic “restrictive filling pattern”-a sharp spike in early filling (E wave) followed by a very short deceleration time (under 150 ms). Cardiac MRI reveals late gadolinium enhancement in a non-coronary pattern, and extracellular volume over 35% confirms scarring. A biopsy is often needed to identify amyloid deposits.
Unlike DCM and HCM, RCM doesn’t respond to standard heart failure drugs. Treatment targets the root cause. For light-chain amyloidosis, drugs like daratumumab or bortezomib are used. Hemochromatosis is treated with regular blood removal (phlebotomy). For transthyretin amyloidosis, tafamidis can slow progression-it improves walking distance by 25 meters in six months, but costs $225,000 a year in the U.S.
Prognosis is the poorest of the three types. Survival rates drop to 30% to 50% at five years, depending on the underlying cause. Many patients need transplants, but the disease often returns if the root condition isn’t controlled. The biggest challenge? Misdiagnosis. RCM looks a lot like constrictive pericarditis-a condition where the sac around the heart hardens. But they require totally different treatments. One needs surgery to remove the sac; the other needs drugs to stop the infiltration.
Why Classification Matters
Doctors used to group all heart muscle diseases together. Now, they know better. The way the heart changes-whether it’s stretched, thickened, or stiff-tells them what’s wrong inside. That changes everything: how they test, what drugs they use, whether they screen families, and whether they consider a transplant.
For example, if you have DCM with a TTN gene mutation, your kids need genetic testing. If you have HCM with an MYBPC3 mutation, you shouldn’t play competitive sports. If you have RCM from amyloidosis, you need a hematologist, not just a cardiologist.
And new tools are changing the game. Cardiac MRI can now spot early fibrosis before symptoms show. Genetic panels test 17 genes at once. CRISPR-based therapies for HCM are entering clinical trials in 2024. Precision medicine is no longer science fiction-it’s in the clinic.
What You Should Know
If you have a family history of sudden cardiac death before age 50, unexplained heart failure, or fainting during exercise, get checked. Many people live with HCM for years without knowing. Routine EKGs and echocardiograms can catch it early.
Don’t ignore fatigue or swelling. If you’ve had chemotherapy or heavy alcohol use, ask your doctor about heart function. And if you’ve been told you have “heart failure” without a clear cause, push for a cardiomyopathy workup. Too many cases are misclassified.
The bottom line? Cardiomyopathy isn’t a single diagnosis. It’s three different diseases that happen to affect the same organ. Understanding which one you’re dealing with isn’t academic-it’s the difference between managing symptoms and saving your life.
Can you have cardiomyopathy without symptoms?
Yes. Many people with hypertrophic cardiomyopathy, especially younger individuals, have no symptoms until they collapse during exercise. Dilated cardiomyopathy can also be silent until heart failure develops. That’s why family screening and routine heart checks are crucial, especially if there’s a history of sudden cardiac death.
Is cardiomyopathy hereditary?
It can be. About 30% to 40% of dilated cardiomyopathy cases and up to 60% of hypertrophic cases have a genetic cause. Restrictive cardiomyopathy is less often inherited, except in rare storage diseases like Fabry disease. Genetic testing is recommended for anyone diagnosed with DCM or HCM, especially if a close relative has been affected.
Can exercise cause cardiomyopathy?
Intense, long-term endurance exercise can rarely lead to a form of dilated cardiomyopathy in susceptible individuals, but it’s not common. More often, exercise reveals an existing condition-especially HCM. Athletes with undiagnosed HCM are at risk of sudden death during exertion. That’s why screening athletes with EKGs and echocardiograms is standard in many countries.
What’s the difference between cardiomyopathy and heart failure?
Cardiomyopathy is a disease of the heart muscle itself. Heart failure is a syndrome-meaning the heart isn’t pumping well enough to meet the body’s needs. Cardiomyopathy often leads to heart failure, but not all heart failure is caused by cardiomyopathy. For example, heart failure can also come from a heart attack or leaky valves.
Are there new treatments on the horizon?
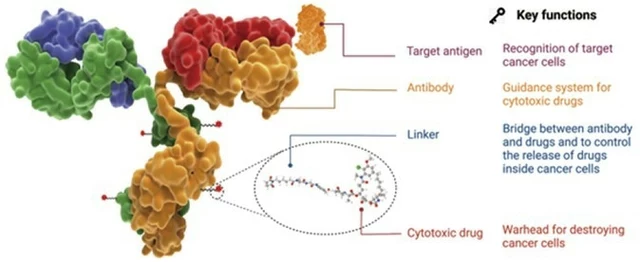
Yes. For HCM, gene-editing therapies like VERVE-201 (targeting MYBPC3 mutations) are in early trials. For amyloidosis-related RCM, new monoclonal antibodies are improving survival. In DCM, gene therapies like AAV1/SERCA2a aim to restore calcium handling in heart cells. These aren’t cures yet, but they represent the first targeted treatments for these conditions.
If you’ve been diagnosed with any type of cardiomyopathy, work with a specialist who understands the nuances. General cardiologists may miss key details. Centers with dedicated cardiomyopathy programs offer better outcomes, genetic counseling, and access to clinical trials. Early, accurate diagnosis doesn’t just improve quality of life-it saves lives.






10 Comments
Kevin Kennett January 29, 2026
Man, I had no idea HCM was the #1 cause of sudden death in young athletes. My cousin collapsed during a college basketball game-no warning, no history. They finally diagnosed him after his dad’s EKG showed the same mutation. If you play sports and have a family history, get checked. Period.
Jess Bevis January 30, 2026
RCM is terrifying. Amyloidosis hits hard and fast.
matthew martin February 1, 2026
So this is what happens when your heart stops being a pump and starts being a drama queen. DCM? It’s like your left ventricle threw a tantrum and stretched out like a balloon animal at a kid’s party. HCM? That’s your heart trying to be a bodybuilder but forgetting it’s not supposed to be that thick. And RCM? Oh, that’s your heart deciding to wear a corset made of rubber and refusing to breathe. I mean-why? Why does the body do this to itself? And why do we still treat it like it’s one disease? We’re not even close to fixing the root causes. We’re just patching the leaks while the whole damn boat sinks.
And don’t even get me started on the price tags. $225k a year for a drug that buys you six extra months? That’s not medicine-that’s a luxury tax on being unlucky. Meanwhile, people are choosing between insulin and their heart meds. This system is broken. We need to stop treating symptoms and start treating the damn biology.
But hey, at least we’ve got CRISPR on the horizon. Maybe in 10 years, we’ll be editing genes like we edit TikTok videos. Until then? Stay off the alcohol. Get screened. And if you’re an athlete? Don’t be a hero. Get checked. Your heart doesn’t care how hard you sprint.
Also-mavacamten? That’s a miracle drug. But only if you’re rich. And that’s not science. That’s capitalism with a stethoscope.
Someone’s gotta say it: medicine’s still playing whack-a-mole with heart disease. We need to stop being reactive and start being predictive. Genetic panels? Great. But they’re useless if no one can afford them. Or if your doctor doesn’t know how to read them.
I’ve seen too many people get misdiagnosed as ‘just fat and out of shape’ when their heart’s already screaming. That’s not negligence. That’s systemic blindness.
And yeah-I’m mad. You should be too.
Jeffrey Carroll February 2, 2026
Thank you for this comprehensive and clinically accurate overview. The distinction between cardiomyopathy and heart failure is frequently misunderstood even among healthcare professionals. The emphasis on genetic screening in familial cases is particularly vital, as early detection can alter the natural history of disease progression significantly. I would encourage all primary care providers to consider referral to a specialized cardiomyopathy center when unexplained ventricular dysfunction is identified.
doug b February 4, 2026
If you’re tired all the time and your legs are puffy, don’t just blame your job or your age. Get your heart checked. Seriously. I ignored it for two years. Ended up in the hospital. Now I’m on meds and I feel like a new person. Don’t wait like I did.
Katie Mccreary February 5, 2026
So… let me get this straight. You’re telling me the reason people die during marathons is because their hearts are genetically defective? And the solution is… more drugs? More expensive drugs? More tests? More paperwork? And the people who can’t afford it just… die? That’s not medicine. That’s a lottery. And you’re the guy selling the tickets.
SRI GUNTORO February 7, 2026
This is what happens when people abandon God’s natural order. The heart was never meant to be tampered with. Modern medicine thinks it can fix everything with chemicals and machines. But God gives us symptoms for a reason. If your heart is failing, maybe it’s because you’ve been living in sin-gluttony, pride, laziness. Pray. Fast. Repent. No drug will heal what your soul has broken.
Rose Palmer February 9, 2026
It is imperative to underscore the significance of multidisciplinary care in the management of cardiomyopathies. The integration of genetic counseling, advanced imaging modalities, and specialized pharmacologic regimens has demonstrably improved prognostic outcomes. Furthermore, the advent of targeted therapies such as mavacamten and tafamidis represents a paradigm shift toward precision medicine, necessitating ongoing collaboration between cardiology, hematology, and molecular diagnostics teams to optimize patient care.
Howard Esakov February 9, 2026
Wow. So I’m basically supposed to believe that my heart is just… broken by my genes? And the only solution is a $200K drug that makes you feel worse? 🤡 I mean, I get it. Pharma’s got us all on a treadmill. But I’d rather just eat avocado toast and hope for the best. 😎
Rhiannon Bosse February 10, 2026
Okay but… what if this is all a lie? What if cardiomyopathy isn’t real? What if it’s just a way to sell MRIs and ICDs? I mean, think about it-every time someone gets diagnosed, the hospital makes millions. And the families? They’re too scared to question it. I read a guy on a forum who said his ‘HCM’ disappeared after he quit sugar and did yoga for 6 months. No one talks about that. Why? Because the system doesn’t want you to know you can heal yourself. 😳