FDA Advisory Panel Recommends Approval of Flibanserin for Female Libido
On June 4, 2015, a significant decision was reached as an advisory committee to the U.S. Food and Drug Administration (FDA) recommended the approval of a groundbreaking new drug aimed at enhancing female libido. The drug, flibanserin, developed by Sprout Pharmaceuticals, is targeted at treating hypoactive sexual desire disorder (HSDD), a condition that affects women by causing a persistent lack of sexual desire. This recommendation came after two prior rejections by the FDA due to questions around the drug's safety and efficacy. The committee’s decision, after detailed discussions weighing the drug’s benefits against its risks, was seen as a milestone in the realm of women's sexual health.
Understanding Hypoactive Sexual Desire Disorder
Hypoactive sexual desire disorder (HSDD) is a condition that has long been underrecognized and underreported. Characterized by a persistent or recurrent absence of sexual fantasies and desire for sexual activity, HSDD affects not only the physical aspect of a woman’s life but also her emotional and psychological well-being. It’s a complex disorder that can stem from numerous factors, including hormonal changes, relationship issues, and psychological factors such as stress and anxiety. The development of flibanserin thus represents a significant step forward in both acknowledging and addressing this often overlooked aspect of women's health.
The Journey of Flibanserin
Flibanserin’s journey to approval was anything but smooth. Originally developed as an antidepressant, its potential for treating HSDD was identified when women participants in clinical trials reported increased sexual desire as a side effect. However, the path to recognition wasn’t straightforward. The FDA had twice rejected the drug due to mixed results in clinical trials and concerns over side effects such as dizziness, nausea, and a potential risk of fainting. But advocates pushed on, arguing that women deserved options for enhancing their sexual health just as men did, with their own range of treatments like Viagra.
A Critical Committee Meeting
The committee meeting on June 4 was a day marked by passionate discussions from all sides. Experts, physicians, and patient advocates presented their cases, debating flibanserin’s potential benefits and the serious concerns about its side effects. Proponents pointed to the lack of other medical treatments available for women suffering from HSDD, highlighting the disparity between the treatments available for men and women’s sexual health issues. The narrative was framed around fairness, equality, and the need to provide women with viable options for improving their sexual well-being.

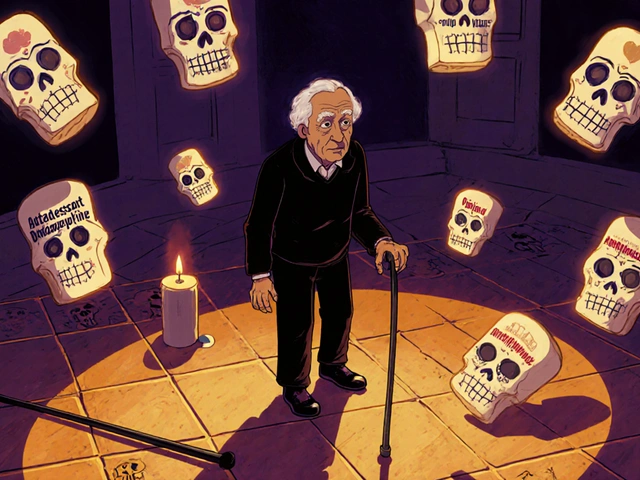
The Mechanism and Restrictions
Flibanserin works by targeting neurotransmitters in the brain, specifically serotonin and dopamine, which are involved in regulating sexual desire and arousal. Unlike male sexual enhancement drugs which primarily address physical symptoms, flibanserin works on the psychological aspects of sexual desire. The FDA, taking into account the advisory committee’s recommendation, approved the drug under the brand name Addyi in August 2015. However, this approval came with stringent restrictions. Addyi is not to be taken with alcohol, due to the risk of severe low blood pressure and fainting, and it’s contraindicated with certain medications. These precautions were deemed necessary to mitigate the potential side effects and ensure patient safety.

A Milestone and a Controversy
The approval of Addyi was hailed as a significant advancement for women's sexual health. Advocates viewed it as a long-overdue recognition of women's needs in the realm of sexual function. The approval also ignited conversations about gender equality in medical research and treatment options. Critics, however, voiced concerns that the decision was influenced by lobbying and advocacy groups rather than based purely on scientific evidence. They questioned whether the drug’s approval had more to do with pressure from outside voices than with conclusive data demonstrating its effectiveness and safety.
An Ongoing Dialogue
The debate surrounding the approval of Addyi continues to spur important dialogues about women's health and medical equity. It has brought attention to the broader issue of how sexual health is approached and addressed, especially for women. The question remains whether the medical community is doing enough to explore and support women-specific health issues without bias or undue influence. As more data and research become available, the ultimate impact of Addyi on women’s health will become clearer, either cementing its place as a breakthrough treatment or prompting further scrutiny and improvements.
The Road Ahead
As Addyi becomes more integrated into the pharmacopeia for treating HSDD, ongoing monitoring and research will be essential. The medical community will need to closely observe the real-world effects of flibanserin, tracking its safety profile and assessing its long-term benefits and risks. Additionally, this case may set a precedent for future treatments aimed at women's sexual health, encouraging pharmaceutical companies to continue innovating in this often-neglected area. The hope is that, ultimately, women will have access to a broader range of safe and effective treatments that address all aspects of their health and well-being.

Conclusion
In conclusion, the FDA’s approval of flibanserin marked a significant moment in the field of women's sexual health. While it brought about much-needed recognition for HSDD and offered a new treatment option, its journey to approval highlighted the complexities and controversies within medical research and gender equality. As the medical community navigates these waters, the ultimate goal remains clear: to understand and address women's health needs with rigorous science, compassion, and equity.







17 Comments
Nick Bercel August 21, 2024
So... they approved a drug that makes you dizzy and can't drink alcohol? Cool. I guess my wife will just have to choose between a glass of wine and a libido. 🤷♂️
Alex Hughes August 23, 2024
Honestly this whole thing is a reflection of how medicine has historically ignored female biology. Men get Viagra and we get told to "just relax" or "talk to your partner". Flibanserin isn't perfect but it's a start. The fact that we're even debating this in 2015 is kind of embarrassing.
Hubert vélo August 24, 2024
They say it's for HSDD but I bet Big Pharma is just pushing this because they realized women spend more on beauty products than men. This is just the beginning. Next they'll sell us mood-altering tampons and antidepressant perfumes. The pharmaceutical-industrial complex is eating us alive.
Kalidas Saha August 25, 2024
OMG THIS IS HUGE!!! 🎉💃 I’ve been waiting for this my whole life!! Finally something that says my desire matters!! 💖🔥 #AddyiRevolution #FemaleLibidoWins
Marcus Strömberg August 25, 2024
This is a textbook case of medicalization of normal human variation. Women aren't broken because they don't want sex every day. This drug pathologizes natural fluctuations in desire. If you're not sexually active, maybe it's not a disorder - maybe it's a sign your life needs adjusting.
Matt R. August 27, 2024
We let a bunch of overeducated liberals in white coats decide what's good for women now? Meanwhile, real men get to take a pill and get hard without being told to avoid alcohol or take it at 11 PM with a full stomach. This is what happens when you give feminism a prescription pad.
Wilona Funston August 27, 2024
I'm a clinical psychologist who's worked with HSDD patients for 18 years. The data is weak, yes - but the lived experience of these women is real. Many have spent years being told it's "all in their head" or that their partner isn't attractive enough. This drug doesn't fix relationships, but it gives some women a biological foothold to start healing. That's worth something.
Ben Finch August 28, 2024
So... you take this pill at night, don't drink, and then... what? You get turned on by your spouse? Or do you just stare at the ceiling wondering why you're not feeling anything? Also, why is it called Addyi? Sounds like a typo for 'add me'.
Naga Raju August 30, 2024
I think this is a good step forward 🙏 Women deserve to feel whole in their bodies. I hope this opens doors for more research. Maybe one day we'll have treatments that don't just target chemistry but also emotional connection 💞
Dan Gut August 30, 2024
The clinical trials demonstrated a statistically insignificant increase in satisfying sexual events - 0.4 more per month compared to placebo. The number needed to treat is 8.3. The risk-benefit ratio is not clinically meaningful. This approval was driven by advocacy, not evidence.
Jordan Corry August 31, 2024
This is the dawn of a new era! 💪 Women, stop apologizing for wanting pleasure! This isn't just a pill - it's a revolution in your right to feel desire without shame. You are not broken. You are not too much. You are not too little. You are enough. And now you have a tool. Use it. Own it. Live it. 🔥
Mohamed Aseem September 1, 2024
They gave women a drug that makes them faint but men get a pill that makes them hard. Classic. This is what happens when you let emotional blackmail dictate science. Men's health has been ignored for decades too - why is this only about women? Hypocrites.
Steve Dugas September 3, 2024
The data is underwhelming. The side effects are severe. The marketing campaign was relentless. This is not medicine. This is commodification of female sexuality under the guise of empowerment. Don't be fooled.
Paul Avratin September 3, 2024
The pharmacological modulation of serotonin-dopamine pathways to restore libido represents a paradigmatic shift in the somatopsychic interface of female sexuality. It's not merely a pharmacological intervention - it's a sociocultural recalibration of embodied desire.
Brandi Busse September 3, 2024
I mean seriously who even has time for this? Take a pill every night don't drink and hope you get in the mood? My husband barely talks to me after work. I'm not taking a pill for that
Colter Hettich September 5, 2024
Flibanserin is the pharmaceutical equivalent of painting a smile on a dead fish. Desire cannot be chemically engineered without addressing the existential vacuum that often underlies its absence. The body is a mirror of the soul - and no pill can heal what the soul refuses to speak.
Prem Mukundan September 7, 2024
This is the first step. But let's not forget: we need better education on sexual health, access to therapy, and less stigma. A pill won't fix a culture that tells women to be quiet about their needs. This is a tool, not a solution.