Drug Interaction Checker
Check Your Medications
Enter medications you're taking to identify potential interactions. Common examples: warfarin, ibuprofen, simvastatin, ketoconazole.
When you take more than one medication, something invisible but powerful is happening inside your body. Two drugs might be working together in ways you never expected-sometimes helping, but often hurting. This isn’t just theoretical. It’s happening right now to millions of people, especially older adults on multiple prescriptions. A simple mix like warfarin and ibuprofen can send someone to the hospital with internal bleeding. Or a common antibiotic like erythromycin combined with a cholesterol drug like simvastatin can trigger muscle damage so severe it leads to kidney failure. These aren’t rare accidents. They’re predictable, preventable, and shockingly common.
What Exactly Is a Drug-Drug Interaction?
A drug-drug interaction (DDI) happens when one medication changes how another one works. This isn’t about allergies or side effects from a single drug. It’s about two or more drugs influencing each other’s behavior in your body. Think of it like traffic on a highway. One car (drug) changes the speed, direction, or exit route of another. The result? Either too much of a drug builds up, or not enough gets where it needs to go.
There are two main types: pharmacokinetic and pharmacodynamic. Pharmacokinetic interactions are about what your body does to the drug-how it absorbs, moves, breaks down, or gets rid of it. Pharmacodynamic interactions are about what the drugs do to your body together-like two painkillers amplifying each other’s effect, or one drug blocking another’s action entirely.
How Your Body Processes Drugs: The Pharmacokinetic Pathway
Your body treats every drug like a visitor. It has to let it in, move it around, break it down, and then kick it out. Each step is a potential point of conflict.
Absorption happens mostly in the gut. Some drugs change stomach acidity or how fast food moves through your intestines. For example, antacids like Tums can make it harder for ketoconazole (an antifungal) to be absorbed, rendering it useless. That’s why you’re told to take certain pills on an empty stomach.
Distribution is about how drugs travel through your bloodstream. Many drugs stick to proteins in your blood, like hitchhikers on a bus. If two drugs compete for the same protein, one can knock the other loose. Warfarin, for instance, is tightly bound to proteins. When you add another drug like sulfonamides (antibiotics), warfarin gets freed up into your bloodstream. Suddenly, your blood thins way more than expected-and bleeding risk spikes.
Metabolism is where most interactions happen. Your liver uses enzymes to break down drugs. The most important family of these enzymes? The cytochrome P450 system, especially CYP3A4. This enzyme handles about half of all prescription drugs. When a new drug comes in, it can either slow down (inhibit) or speed up (induce) this enzyme.
Take simvastatin, a statin used to lower cholesterol. It’s broken down by CYP3A4. Now add ketoconazole, a strong inhibitor of that enzyme. Simvastatin can’t be processed. It piles up. Concentrations can jump 10 to 20 times higher. That’s not just a side effect-it’s a red flag for rhabdomyolysis, a condition where muscle tissue breaks down and can shut down your kidneys. The FDA has issued multiple warnings about this combo.
On the flip side, St. John’s Wort, a popular herbal supplement for mild depression, is a powerful inducer of CYP3A4. It can slash the effectiveness of birth control pills, transplant drugs like cyclosporine, and even some HIV medications by up to 60%. People don’t realize they’re taking a drug at all-just a “natural remedy.”
Excretion is the final step. Your kidneys and liver flush out drug leftovers. Some drugs block the transporters that move drugs out. For example, verapamil, used for high blood pressure, blocks a transporter called P-glycoprotein. When taken with digoxin (a heart medication), digoxin builds up to toxic levels. That can cause dangerous heart rhythms. This isn’t rare-it’s documented in over 500 case reports.
When Drugs Talk Directly: Pharmacodynamic Interactions
These don’t change drug levels. They change what the drugs do to your body-when they’re already there.
Synergistic interactions mean the effects add up. Take benzodiazepines (like lorazepam) and opioids (like oxycodone). Both depress the central nervous system. Together, they can slow breathing to a dangerous level. That’s why the FDA requires black box warnings on these combinations.
Antagonistic interactions mean one drug cancels out the other. For example, beta-blockers lower blood pressure. NSAIDs like ibuprofen can block that effect, making blood pressure control harder. That’s why doctors warn heart patients not to use OTC painkillers casually.
One of the most deadly pharmacodynamic combos? Fluoroquinolones (like ciprofloxacin) and macrolides (like azithromycin). Both can prolong the QT interval on an ECG. Alone, they’re usually safe. Together? The risk of torsades de pointes-a chaotic, life-threatening heart rhythm-goes up by 5.7 times. This isn’t a guess. It’s backed by clinical data from the FDA and European regulators.

Who’s Most at Risk?
You don’t need to be a doctor to know who’s most vulnerable. It’s the people taking the most drugs.
Older adults-especially those over 65-are the biggest group. The average person in this group takes four to five prescription drugs. Add over-the-counter meds, vitamins, and supplements? That’s often seven or more. The Beers Criteria, updated in 2019, lists 30 high-risk combinations for seniors. One of the top ones? NSAIDs + anticoagulants. This combo triples or quadruples the risk of major bleeding. And it’s still prescribed all the time.
People with chronic conditions-heart disease, diabetes, HIV, epilepsy-are also at high risk. Their meds are often narrow-therapeutic-index drugs. That means the difference between the right dose and a toxic dose is tiny. Warfarin is a classic example. A 20% change in its level can mean the difference between clotting and bleeding.
Genetics play a role too. About 5% of people are poor metabolizers of CYP2D6. If they take codeine, which needs CYP2D6 to turn into morphine, they get no pain relief. But if they’re ultrarapid metabolizers? They turn codeine into morphine too fast. Add a CYP3A4 inhibitor like clarithromycin? Morphine levels spike. That’s how a simple painkiller turned into an overdose.
How Are These Interactions Caught?
Drug companies test for interactions during development. They use human liver cells, microsomes, and healthy volunteers to measure how a new drug affects or is affected by others. The FDA and EMA require this before approval.
But real-world use is messier. That’s why databases exist. The Liverpool HIV-Drug Interactions Checker updates daily and covers over 350 antiretroviral combos. Pharmacists use it. Doctors use it. It’s not just a tool-it’s a lifeline.
Electronic health records (EHRs) have DDI alerts. But here’s the problem: they’re noisy. Studies show 80-90% of alerts are false. Clinicians get overwhelmed. They start ignoring them. That’s called alert fatigue. One study found doctors override 96% of alerts. That’s not negligence-it’s burnout.
Some systems are getting smarter. Epic’s “Suggestive Warnings” feature, rolled out in 2021, doesn’t just say “warning.” It says, “This combo increases bleeding risk by 4x in patients over 70. Consider celecoxib instead.” That’s context. That’s useful.
What Can You Do?
You don’t need to memorize enzyme pathways. But you can take control.
- Keep a full list of everything you take: prescriptions, OTCs, vitamins, herbs, supplements. Even “just aspirin.”
- Ask your pharmacist every time you get a new prescription: “Could this interact with anything else I’m taking?” Pharmacists caught 37% fewer DDIs in one study just by reviewing regimens.
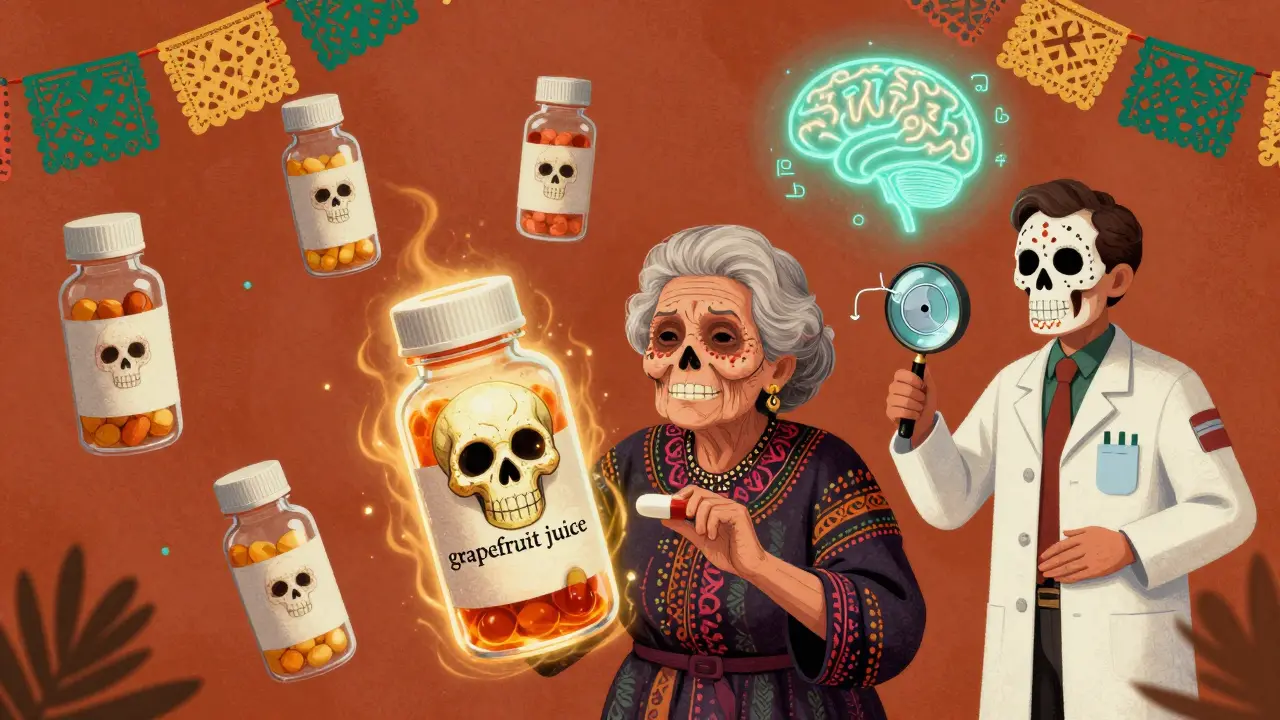
- Don’t assume natural = safe. St. John’s Wort, grapefruit juice, garlic supplements-they all interact. Grapefruit juice can make some statins 5x more potent. One glass can do it.
- Know your high-risk drugs. Warfarin, digoxin, lithium, theophylline, cyclosporine, and some antidepressants need close monitoring. If you’re on one, ask about regular blood tests.
- Use one pharmacy. It lets your pharmacist see your full history. They’ll flag risks you didn’t even know existed.
The Future: Personalized Medicine and AI
The next big leap? Tailoring drug choices to your genes and your habits.
The Clinical Pharmacogenetics Implementation Consortium (CPIC) has published 22 guidelines. One says: don’t give codeine to CYP2D6 ultrarapid metabolizers. Another says: avoid certain antidepressants if you’re a CYP2C19 poor metabolizer.
And then there’s AI. In 2021, a machine learning model trained on 89 million electronic health records predicted DDIs with 94.8% accuracy. It didn’t rely on rules like “CYP3A4 inhibitor + substrate = bad.” It learned from real patient outcomes. That’s the future: not just alerts, but predictions.
But even AI can’t replace the human touch. A 2022 study found that patients who had a 5-minute conversation with their pharmacist about interactions had 30% fewer hospital visits. That’s not technology. That’s care.
Bottom Line
Drug-drug interactions aren’t mysteries. They’re predictable, measurable, and preventable. But they require attention. Every pill you take has a story. When you stack them, those stories start to overlap. Sometimes they reinforce each other. Sometimes they collide.
The goal isn’t to avoid all combinations. It’s to know which ones matter. And to make sure your care team does too.








12 Comments
Karianne Jackson February 8, 2026
I took ibuprofen with my blood thinner and almost died. Like, I woke up with my arm covered in bruises and thought I got mugged. Turned out my doctor didn’t even know they interacted. 🤯 #WTFMedicine
Joseph Charles Colin February 9, 2026
The CYP3A4 inhibition cascade is a well-documented pharmacokinetic phenomenon, particularly with statins and macrolides. The area under the curve (AUC) for simvastatin can increase by 10- to 20-fold, exceeding the therapeutic index and precipitating rhabdomyolysis. This is why pharmacogenomic screening for CYP polymorphisms is now included in institutional protocols.
Randy Harkins February 9, 2026
This is so important. 💙 I’m so glad someone broke this down clearly. My grandma was on 7 meds and never knew half of them were fighting each other. She ended up in the hospital from a warfarin-ibuprofen combo. Now she uses one pharmacy, keeps a handwritten list, and her pharmacist checks everything. It’s not fancy, but it saved her life. 🙏
Tori Thenazi February 10, 2026
Wait... so you’re telling me the FDA *knows* this happens... and still lets drug companies sell these combos?! And your EHR alerts are ‘noisy’? 😒 That’s not ‘noisy’-that’s corporate negligence. Big Pharma doesn’t want you to know how dangerous polypharmacy is. They profit off the chaos. And don’t even get me started on St. John’s Wort being labeled ‘natural’-it’s a biochemical bomb. 🕵️♀️💊
Frank Baumann February 10, 2026
I’ve been on 11 medications for 8 years now. I used to think I was just ‘sickly’-turns out I was just being slowly poisoned by my own pharmacy. I found out my antidepressant was blocking my thyroid med because my doctor didn’t check interactions. I had to beg my pharmacist to run a full review. She found 6 high-risk combos I didn’t even know about. One of them was grapefruit juice with my blood pressure pill. I drank it every morning. I’m lucky I’m still here.
Alex Ogle February 11, 2026
I’m a nurse. I see this every day. The worst part? Patients don’t tell you about their supplements. ‘Oh, I just take turmeric for my knees.’ Yeah, turmeric inhibits CYP2C9 and P-gp. That’s gonna mess with your warfarin. And they never mention OTCs. ‘I only take Tylenol.’ Right. And I’m the Queen of England. We need better systems. But also-patients need to speak up. Even if it feels awkward.
Brandon Osborne February 11, 2026
I don’t get why people are surprised by this. You think your body is some magical little sandbox where drugs play nice? Nah. It’s a war zone. And the drug companies? They’re the generals. They don’t care if you bleed out-they care if you keep buying pills. And don’t even get me started on ‘natural remedies.’ That’s just snake oil with a yoga vibe. 🤬
Lyle Whyatt February 12, 2026
I live in Australia and we’ve got the PBS (Pharmaceutical Benefits Scheme) that flags interactions at the pharmacy counter. It’s not perfect, but it’s way better than the US system. I had a friend on warfarin who started taking omeprazole-no one told her it increases INR. She almost had a stroke. Now her pharmacist calls her every time a new med is added. It’s simple. It’s cheap. It works. Why can’t we just do this everywhere?
Random Guy February 13, 2026
so like… if i take my adderall and my weed and my energy drink and my protein powder… is that a ddi or just my life?
Sam Dickison February 15, 2026
The P-glycoprotein transporter point is huge. Verapamil + digoxin is a classic, but most docs don’t even check for it anymore. I’ve seen patients crash because they got a new script for diltiazem and no one adjusted the digoxin dose. It’s not rocket science-it’s basic pharmacokinetics. But yeah, alert fatigue is real. We need smarter systems, not more pop-ups.
Chelsea Cook February 15, 2026
I love that you mentioned the pharmacist. Like, seriously-your pharmacist knows more about your meds than your doctor does. I used to think they just handed out pills. Then I asked one, ‘Hey, does this interact with my fish oil?’ She paused. Then said, ‘You’re on warfarin. Fish oil can increase bleeding risk. Also, your garlic supplement? Double whammy.’ I didn’t even know I was taking garlic. She had to pull up my 14-month history. That’s a hero.
Andy Cortez February 16, 2026
AI predicting DDIs with 94% accuracy? Lmao. You think the algorithm doesn’t get trained on data from pharma-funded trials? The whole system’s rigged. They don’t want to fix this-they want to sell you more tests, more apps, more ‘personalized’ meds. Meanwhile, your grandma’s on 8 pills and no one’s looking at the whole picture. Just sayin’.