Osteoporosis: How to Spot It Early and Keep Your Bones Strong
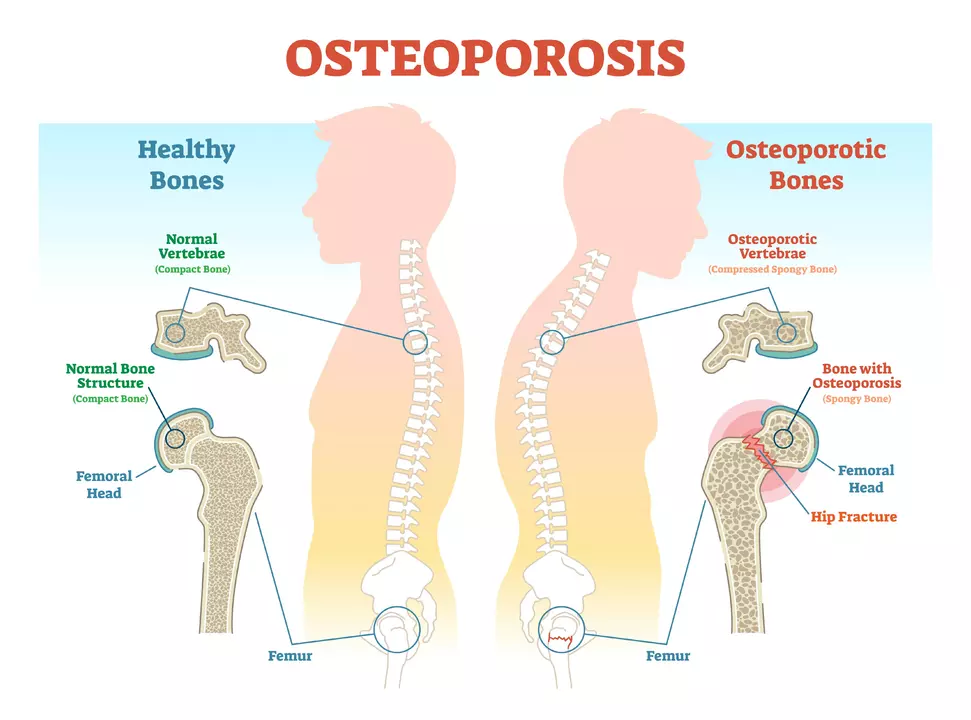
If you’ve heard the word "osteoporosis" but aren’t sure what it really means, you’re not alone. In plain terms, osteoporosis is a condition where bones become porous and fragile, making even minor falls risky. The good news? You can catch it early and take steps to slow—or even stop—its progress.
Spotting Osteoporosis Early
The first clue often shows up as a silent loss of bone density. Most people don’t feel any pain until a fracture occurs, usually in the wrist, hip, or spine. If you’re over 50, have a family history of broken bones, or take steroids for a long time, get a bone mineral density (BMD) test. It’s quick, painless, and gives doctors a clear picture of your bone health.
Other red flags include a sudden loss in height, a curved posture, or back pain that doesn’t go away. These signs can signal vertebral fractures—tiny cracks in the spine that happen without any big injury. When you notice them, call your doctor right away for an X‑ray or CT scan.
Protecting Your Bones
Diet is a cornerstone of bone health. Aim for at least 1,200 mg of calcium daily—think dairy, leafy greens, fortified plant milks, and almonds. Pair calcium with vitamin D (about 800–1,000 IU) so your body actually absorbs the mineral. Sunlight, fatty fish, and supplements can help you hit that target.
Exercise matters too. Weight‑bearing activities like brisk walking, dancing, or light jogging send a signal to bone cells to stay strong. Add resistance training—using bands or dumbbells—twice a week to boost muscle support around your skeleton.
If lifestyle tweaks aren’t enough, medication can make a difference. Bisphosphonates are the most common prescription; they slow bone loss and lower fracture risk. Other options include denosumab injections, selective estrogen receptor modulators (SERMs), or newer anabolic agents that actually build new bone. Talk to your doctor about which one fits your health profile.
Don’t forget habits that can hurt bone density. Smoking and heavy drinking both accelerate bone loss. Cutting back on caffeine and avoiding excessive soda also helps, as those drinks can leach calcium from the bones.
Finally, stay on top of regular check‑ups. Even if you’re feeling fine, a yearly BMD test after age 65 (or earlier if you have risk factors) keeps you informed and lets your doctor adjust treatment before a break happens.
Osteoporosis might sound scary, but with the right mix of screening, nutrition, exercise, and medical care, you can protect your bones for years to come. Keep an eye on warning signs, make small daily changes, and partner with your healthcare team—you’ve got this!
- Archer Pennington
- 14
The Benefits of Tai Chi for Osteoporosis Patients
I just learned about how beneficial Tai Chi can be for osteoporosis patients. This ancient Chinese practice not only improves balance and flexibility, but it can also help to strengthen bones and reduce the risk of fractures. The slow, gentle movements are perfect for those with osteoporosis, as they put minimal stress on the joints. Plus, Tai Chi has been shown to improve overall mental well-being and reduce stress, which is essential for managing this condition. I highly recommend giving Tai Chi a try if you're dealing with osteoporosis - your body and mind will thank you!
Read more- Archer Pennington
- 13
The Relationship Between Osteoporosis and Kidney Disease
As a blogger, I've recently come across an interesting connection between osteoporosis and kidney disease. Osteoporosis is a condition where our bones become weak and brittle, while kidney disease affects our kidneys' ability to filter waste from our blood. It turns out that these two conditions are closely linked, as kidney disease can lead to an imbalance in the minerals needed for bone health. This can result in a higher risk of developing osteoporosis for those suffering from kidney disease. It's essential for people with kidney issues to monitor their bone health and take necessary precautions to prevent or manage osteoporosis.
Read more