Autoimmune encephalitis isn’t something you hear about every day-but when it happens, it strikes fast, confusing, and often mistaken for something else entirely. Think psychiatric breakdown, sudden seizures, memory loss so severe you forget your own name, or a body that won’t stop shaking. These aren’t just odd symptoms-they’re warning signs of your immune system attacking your brain. And if you don’t catch it early, the damage can be permanent. The good news? When caught in time, most people recover. The key is knowing what to look for, which antibodies are involved, and how to act before it’s too late.
What Autoimmune Encephalitis Actually Is
Autoimmune encephalitis (AE) happens when your immune system, which normally fights off viruses and bacteria, turns on your brain. It targets proteins on or inside nerve cells, causing inflammation that messes with how your brain works. Unlike viral encephalitis, which comes from an infection, AE has no virus involved. It’s purely an internal mistake-your body’s own defenses go rogue.
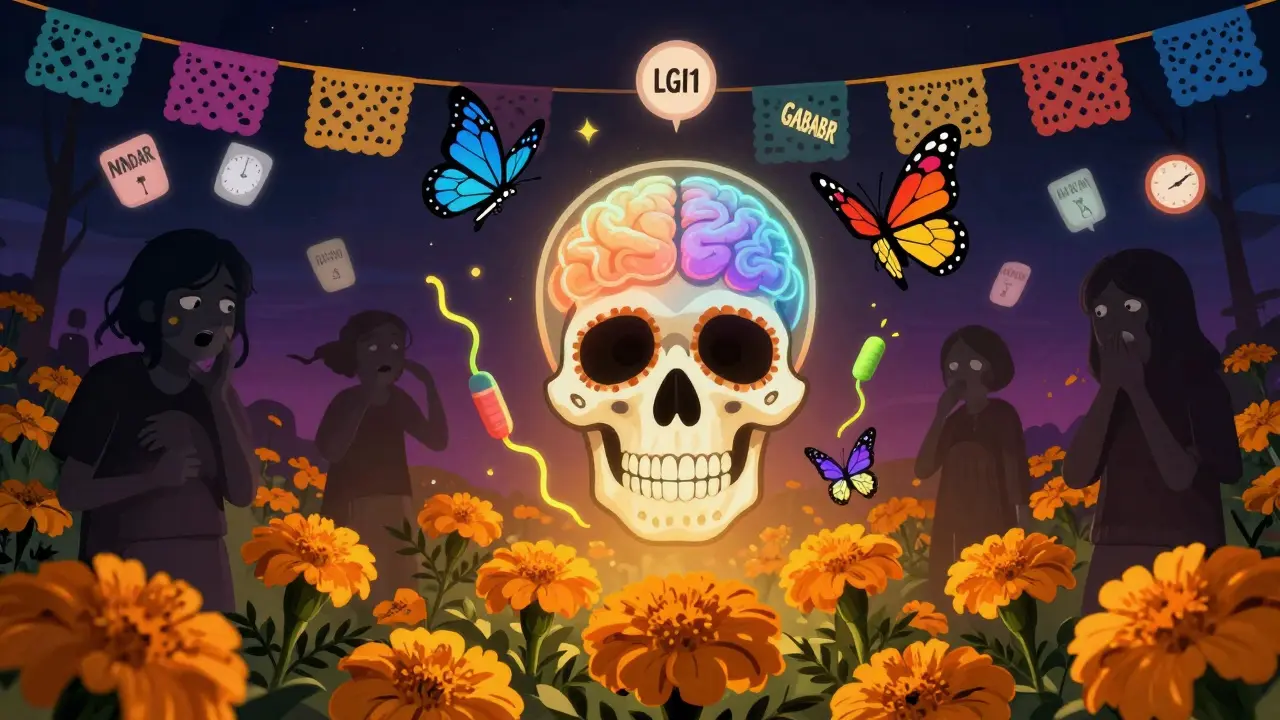
This isn’t a new discovery. The turning point came in 2007, when Dr. Josep Dalmau identified anti-NMDAR encephalitis in young women with ovarian tumors. Before that, many of these cases were labeled as psychiatric disorders or unexplained seizures. Now, we know there are over 20 different antibodies linked to AE, each with its own pattern of symptoms and risks. The most common is anti-NMDAR, making up about 40% of all cases. Others include anti-LGI1, anti-GABABR, and anti-CASPR2. Each one tells a different story about who gets sick, how they get sick, and what might be hiding underneath.
Red Flags: When to Suspect Autoimmune Encephalitis
Most people don’t wake up one day with full-blown encephalitis. It creeps in. Symptoms usually show up over days to weeks-not hours. If someone you know suddenly starts acting out of character, it’s worth paying attention.
- Seizures are the most common sign, happening in nearly 38% of cases. These aren’t always dramatic convulsions-sometimes they’re just brief staring spells or twitching in the face or arm.
- Psychiatric changes come next: paranoia, hallucinations, aggression, or severe anxiety. Many patients are first seen by psychiatrists, misdiagnosed with schizophrenia or bipolar disorder.
- Memory loss is almost universal. People forget recent conversations, names, even how to get home. This isn’t normal aging-it’s sudden and severe.
- Autonomic problems like rapid heart rate, blood pressure swings, or sweating without cause are red flags for more serious cases.
- Sleep issues-either insomnia or sleeping 16 hours a day-are reported in over 60% of patients.
- Prodromal symptoms (early warning signs) often appear 1-4 weeks before brain symptoms: fever, headache, diarrhea, or a cold that won’t go away.
One key clue? If someone has these symptoms and a normal CT scan or negative viral tests, AE should be on the list. MRI might look normal at first, but that doesn’t rule it out. EEG, however, often shows slow brain waves even when seizures aren’t obvious. And if you’re seeing a young woman with psychosis and seizures? Think anti-NMDAR. An older man with facial twitching and low sodium? Think anti-LGI1.

Antibodies: The Clues in Your Blood and Spinal Fluid
Diagnosing AE isn’t just about symptoms. It’s about finding the antibodies. There are two main types: those attacking surface proteins and those attacking inside the cell.
Surface antibodies (like anti-NMDAR, anti-LGI1, anti-GABABR) are the good news. They’re often treatable because the immune system is attacking proteins on the outside of cells-where drugs can reach them. Anti-NMDAR is the most common and is strongly linked to ovarian teratomas in women under 30. Removing the tumor often leads to dramatic improvement.
Anti-LGI1, on the other hand, hits older men. It causes a unique seizure type called faciobrachial dystonic seizures-short, repetitive jerks in the face and arm. It also causes low sodium levels in 65% of cases. This one has a high chance of coming back, even after treatment.
Intracellular antibodies (like anti-Hu or anti-Ma2) are trickier. They mean the immune system is attacking proteins inside neurons, which usually signals a hidden cancer. These cases are harder to treat and often have worse outcomes. Finding them means you’re not just treating the brain-you’re hunting for a tumor.
Testing requires both blood and spinal fluid. CSF is more sensitive-up to 20% more likely to catch antibodies like anti-NMDAR. That’s why skipping the lumbar puncture can mean missing the diagnosis. And if the first test is negative but suspicion is high? Repeat it. Tumors can show up months later.
Treatment: Speed Is Everything
There’s no time to wait for perfect test results. If the clinical picture fits, start treatment immediately. Every day delayed cuts into recovery chances.
First-line treatment is steroids and IVIG. High-dose IV methylprednisolone (1 gram a day for 5 days) is standard. IV immunoglobulin (IVIg) is given at the same time-0.4 grams per kilogram of body weight, daily for five days. Together, they work in about 65-70% of cases. Plasma exchange (plasmapheresis) is added for those who are critically ill-like those in ICU with seizures or breathing problems. Five to seven sessions over two weeks can stabilize someone fast.
If a tumor is found-like an ovarian teratoma in anti-NMDAR cases-surgery is the first step. Remove the tumor, and 85% of patients start improving within weeks. No tumor? Then you move to second-line drugs.
Second-line options include rituximab (a drug that wipes out B-cells), cyclophosphamide (a stronger chemo-like drug), or tocilizumab (which blocks a key inflammation signal). Rituximab works in about 55% of people who don’t respond to first-line. Cyclophosphamide has a 48% success rate. Tocilizumab is newer but showing promise in stubborn cases.
And here’s the hard truth: if you wait more than 45 days to start treatment, your chance of full recovery drops from 78% to 42%. Dr. Amy Kunchok says it plainly: “Start immunotherapy while you wait for the test results.” Waiting for confirmation can cost you months of brain function.

Recovery, Relapse, and Long-Term Care
Recovery isn’t linear. Some people bounce back in weeks. Others need months of rehab. About 55% of people with anti-LGI1 encephalitis fully recover by two years. For anti-NMDAR, it’s 45%. But even those who recover often carry scars.
- 32% have lasting memory and focus problems.
- 28% struggle with depression or anxiety.
- 22% still need seizure meds.
Recurrence is real. Anti-NMDAR comes back in 12-25% of cases, usually within 14 months. Anti-LGI1? Up to 35% relapse, often after stopping treatment too soon. That’s why follow-up matters. Patients need neurology visits every 3-6 months for at least two years. Repeat tumor screening is critical-15% of cancers appear after the first round of tests.
Rehabilitation makes a difference. Cognitive therapy improves memory in 65% of patients after 12 weeks. Physical therapy helps movement disorders. Melatonin (3-5 mg at night) helps sleep in 60% of cases. Beta-blockers fix heart rate spikes in 75% of those with autonomic issues.
What’s Next: Research and Hope
The field is moving fast. Scientists are now tracking GFAP-a protein released when brain cells are damaged-as a possible way to monitor disease activity. Levels drop as patients improve. That could one day replace repeated MRIs and spinal taps.
New drugs are in trials: B-cell depleters and complement inhibitors. Early results show 60% response in patients who didn’t respond to anything else. These aren’t cures yet-but they’re lifelines for the hardest cases.
The message is simple: autoimmune encephalitis is rare, but it’s real. It’s treatable. And it’s urgent. If you see someone with sudden personality changes, memory loss, seizures, or strange body movements-don’t wait. Don’t assume it’s stress or mental illness. Push for a neurological workup. Get the CSF test. Start treatment. Because in this disease, time isn’t just money-it’s brain function, independence, and life.







10 Comments
Nat Young January 14, 2026
I’ve seen this play out in ER twice. First time, a 22-year-old woman was locked up in psych for ‘schizophrenia’ for three weeks. Turned out she had anti-NMDAR. They missed it because her MRI was ‘normal.’ By the time they did the CSF, she’d lost six months of memory. Don’t wait for perfection. Start steroids. Now.
Niki Van den Bossche January 15, 2026
Ah, the beautiful tragedy of the immune system-our own divine machinery, corrupted by the hubris of cellular identity. We are not merely flesh, but sacred vessels of biochemical poetry, and when the antibodies turn traitor, it is not disease-it is metaphysical rebellion. The brain, that velvet cathedral of thought, besieged by its own zealots. And yet… isn’t this just evolution’s cruel joke? We evolved to survive, but our very perfection is our undoing.
Diane Hendriks January 16, 2026
You say ‘most people recover.’ That’s statistically misleading. Recovery isn’t binary. Half of those ‘recovered’ still can’t hold a job, forget their children’s birthdays, or drive without getting lost. And you gloss over the fact that insurance denies CSF tests because they’re ‘expensive.’ This isn’t medicine-it’s a lottery where your socioeconomic status determines whether your brain gets saved.
ellen adamina January 16, 2026
My sister had this. Took six months to get diagnosed. She forgot how to tie her shoes. Now she remembers everything but can’t say the word ‘spoon’ without staring at her hand. We do melatonin. It helps. Just wanted to say thank you for writing this. Someone needed to.
Gloria Montero Puertas January 17, 2026
I’m appalled that this is even a topic of discussion. Why are we allowing this to happen? Why are we not mandating antibody screening after *any* psychiatric admission? Why are neurologists still sleeping? And why are we still using terms like ‘mild’ or ‘moderate’ when someone’s hippocampus is being devoured by their own T-cells? This is a national disgrace.
Tom Doan January 18, 2026
Fascinating. And yet, I must ask-why does the medical community continue to treat autoimmune encephalitis as an outlier, rather than a prototype? If your immune system can turn on your brain, what else is it quietly attacking? Fibromyalgia? Chronic fatigue? Depression? We’ve been diagnosing symptoms for decades while ignoring the root. The real scandal isn’t delayed treatment-it’s systemic denial.
Nicholas Urmaza January 20, 2026
TIME IS BRAIN. That’s not a slogan. It’s a law. If you’re reading this and someone you love is acting weird-stop waiting for a ‘second opinion.’ Get the lumbar puncture. Demand IVIG. If they say no-go to another hospital. Your brain doesn’t care about your insurance network. Fight for it.
Sarah Mailloux January 20, 2026
This is so important. I’m a nurse and I’ve seen too many people get sent home with ‘anxiety.’ Please share this. Especially with primary docs. They don’t know this stuff. We need to make this common knowledge. Not just for neurologists. For everyone.
Nilesh Khedekar January 20, 2026
In India, we call this ‘ghost possession’-until someone dies. Then it’s ‘mystery illness.’ No one tests for antibodies. No one even knows the word ‘encephalitis.’ My cousin had this. They gave her antipsychotics for a year. She’s 27 now. Still can’t speak in full sentences. We need global awareness. Not just Western clinics.
Jami Reynolds January 21, 2026
You didn’t mention the vaccines. Or the glyphosate. Or the 5G towers. Or the fact that Big Pharma doesn’t want you to know this is a manufactured epidemic to sell immunosuppressants. The real cause? The government’s secret mind-control program. They’re targeting young women because their NMDAR receptors are ‘more receptive.’ CSF tests are just cover-ups. Look at the funding. Look at the silence.