Every year, over 1.5 million people in the U.S. are harmed by medication errors - and most of them happen at home, not in hospitals. If you’re caring for an aging parent, a child with special needs, or someone with chronic illness, you’re likely managing multiple pills, liquids, patches, and injections. One wrong dose, one missed timing, one unclear label - and you could be looking at a hospital trip, a fall, a stroke, or worse. The good news? Most of these errors are preventable. You don’t need to be a nurse. You just need the right system.
Start with a Complete Medication List
The first step in keeping someone safe is knowing exactly what they’re taking. Not just the names - but the full details. That means writing down:- Brand name and generic name (e.g., lisinopril vs. Zestril)
- Exact dosage (5 mg, not just "one pill")
- How often (twice daily, every 8 hours, only at bedtime)
- Why they’re taking it (for blood pressure, for pain, for sleep)
- Any side effects you’ve noticed (dizziness, nausea, confusion)
This list isn’t a one-time task. Update it every time a doctor changes a prescription - even if it’s just a dose tweak. Keep a printed copy in your wallet and another in a folder at home. Share it with every pharmacist, ER doctor, or specialist your loved one sees. Studies show caregivers who keep a full list reduce medication errors by 52%. That’s not a small number. It’s life-changing.
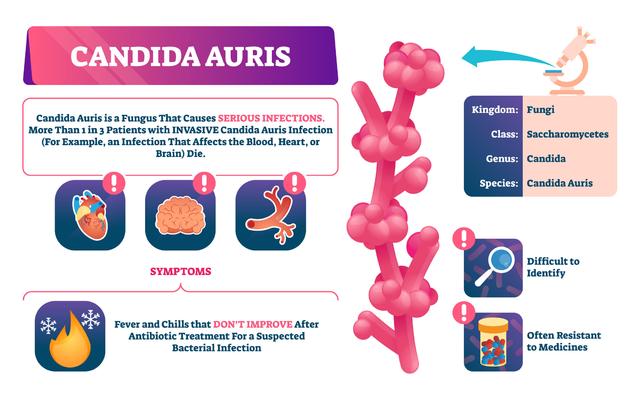
Watch Out for Polypharmacy
If your loved one takes five or more medications daily, they’re in the high-risk group. That’s called polypharmacy. And it’s not just about quantity - it’s about dangerous combinations. The Beers Criteria, updated annually by the American Geriatrics Society, lists 30 drugs that should be avoided in older adults because they cause more harm than benefit. Common offenders include:- Benzodiazepines (like diazepam or lorazepam) - increase fall risk and confusion
- Proton pump inhibitors (like omeprazole) - long-term use linked to bone loss and infections
- Anticholinergics (like diphenhydramine in Benadryl) - cause memory problems and dry mouth
Dr. Michael Steinman’s research at UCSF found nearly half of older adults take at least one drug that’s riskier than helpful. Don’t assume every prescription is necessary. Ask the doctor: "Is this still needed?" and "Are there safer alternatives?"
Use the Right Tools - No Guesswork
Household spoons are dangerous. A tablespoon isn’t the same as a teaspoon. A 2021 study in JAMA Pediatrics showed household spoons vary by 20% to 40% in volume. That’s not a tiny difference - it’s a toxic overdose risk.Always use a calibrated oral syringe for liquids. They’re cheap, easy to find at pharmacies, and labeled in milliliters. For pills, use a seven-day pill organizer with AM/PM compartments. For people with dementia or memory loss, these aren’t optional - they’re essential. The Alzheimer’s Association recommends them as a baseline safety measure.
And don’t forget alarms. Many caregivers on Reddit and ALZConnected say the biggest win was using a pill organizer with built-in alarms. One caregiver wrote: "I set it to beep at 8 a.m. and 8 p.m. My mom used to forget half her meds. Now she takes them on time, every time. It’s the only thing that worked."
Know the High-Risk Mistakes
Some errors happen over and over - and they’re easy to avoid if you know what to watch for.- Look-alike, sound-alike drugs: Hydroxyzine (for allergies) vs. hydrocortisone (for skin). One letter off. Big difference. Always read the label twice.
- Unit confusion: mg vs. mcg. A 1000 mcg dose isn’t the same as 1000 mg - it’s 1,000 times smaller. Pharmacies now print "mcg" clearly, but you should double-check.
- Transitions: 62% of errors happen when someone moves from hospital to home. Ask for a full medication review before discharge. The CARE Act, now law in 47 states, requires hospitals to teach caregivers how to manage meds before letting patients go home.
One caregiver shared how her mother came home from the hospital on five new drugs. She didn’t know why any of them were given. She called the pharmacy - and found two were duplicates. One was an old prescription still on the list. That mistake could have caused a dangerous drop in blood pressure.

Store Medications Right
Medications aren’t like canned food. Heat, moisture, and light can ruin them. Most pills should be stored at room temperature - between 68°F and 77°F. Don’t keep them in the bathroom cabinet. The steam from showers degrades medicine. Don’t leave them in the car in summer. Don’t store insulin in the freezer.Check expiration dates every week. The FDA says 90% of caregivers don’t. Expired antibiotics can become ineffective. Expired epinephrine auto-injectors may not work in an emergency. Set a reminder on your phone: "Check meds - every Sunday."
Use Technology - But Know the Limits
Digital tools like Medisafe and CareZone help 32% of caregivers avoid missed doses. They send alerts, track refills, and let you share updates with other family members. But not everyone is tech-savvy. A National Institute on Aging focus group found 27% of caregivers over 65 find apps frustrating.If tech isn’t your thing, don’t force it. Use a paper calendar with colored pens. Write the time next to each pill. Put sticky notes on the fridge. The goal isn’t to be high-tech - it’s to be consistent.
But if you’re open to it, try one feature: QR code labels. Since May 2023, the CDC has encouraged pharmacies to put QR codes on prescription bottles. Scan it with your phone - and you’ll get dosage info, side effects, and refill reminders. It’s free. Ask your pharmacist if they offer it.
Build a Relationship with Your Pharmacist
Pharmacists are the hidden heroes of medication safety. They see every prescription, every interaction, every red flag. But most caregivers never ask them for help.Go to the pharmacy with your medication list. Ask for a Medication Therapy Management (MTM) review. It’s free for Medicare Part D beneficiaries taking eight or more meds. Even if you don’t qualify, most pharmacists will do a quick check for free. In 2022, pharmacists caught potential problems in 35% of these visits.
One caregiver on FamilyCaregiver.org said: "I asked the pharmacist to check for interactions. She found three dangerous combos I didn’t know about. One was mixing a blood thinner with a common herbal supplement. That could have killed him."

Plan for Regular Check-Ins
Medication safety isn’t a one-time setup. It’s an ongoing job. Set up a 45-minute appointment every six months with a pharmacist. Bring all bottles, including supplements and over-the-counter drugs. Ask: "Is this still needed?" "Is there a safer option?" "Are any of these conflicting?"That’s it. No extra cost. No special skills. Just time. And it cuts adverse drug events by 28%.
Also, spend 10 minutes each week checking:
- Are all pills still in the bottle?
- Are any expired?
- Is the pill organizer full?
- Did the pharmacy send the right refill?
This small habit prevents 18% of pediatric errors - and it works just as well for adults.
What to Do If You Spot a Problem
If your loved one seems confused, dizzy, unusually sleepy, or has a rash after starting a new med - don’t wait. Call the doctor or pharmacist immediately. Don’t assume it’s "just aging." It might be a reaction.Keep a log: Date, time, symptom, what med was taken. That helps the doctor decide fast. In emergencies, call 911. But most problems aren’t emergencies - they’re mistakes. And they’re fixable.
Final Thought: You’re the Last Line of Defense
Hospitals, doctors, and pharmacies make mistakes. That’s human. But you’re the one who sees the pills every day. You notice when the bottle is empty too soon. You hear when your loved one says, "I don’t feel right." You’re the one who catches the error before it becomes a crisis.You don’t need to be perfect. You just need to be careful. Use the list. Use the syringe. Ask the pharmacist. Check the dates. Set the alarm. It’s not complicated. It’s just consistent.
And that consistency? It saves lives.






9 Comments
Shae Chapman December 31, 2025
OMG this hit me right in the feels 😭 I’ve been managing my mom’s 12 meds for 3 years and I didn’t even know about QR codes on bottles-just got one scanned today and it literally showed me she was double-prescribed a blood thinner. THANK YOU for this. I’m printing the list right now and setting up alarms. You just saved her life 🙏💊
Nadia Spira January 1, 2026
Let’s be real-this is just another feel-good checklist for people who don’t understand systemic healthcare collapse. You think a pill organizer fixes Medicare’s $300B waste? The real problem is pharma lobbying, not your ‘lazy’ caregiver forgetting to check expiration dates. Stop moralizing poverty and prescribe policy reform instead. 🤷♀️
henry mateo January 2, 2026
im not a nurse but i read this whole thing and cried a little. my dad took 8 pills a day and i thought he was just ‘getting old’ when he got confused. turns out it was the benadryl. we switched him to melatonin and he’s been lucid for months now. thanks for writing this. i’ll start using the syringe too. i’ve been using a soup spoon… yikes.
Kunal Karakoti January 3, 2026
The philosophical underpinning here is beautiful: agency in the face of institutional failure. We are not merely caretakers-we are epistemic agents reconstructing medical coherence from fragmented systems. The pill organizer becomes a phenomenological anchor, a ritual of dignity against entropy. Yet, one must ask: does this individualized labor absolve the state of its responsibility? Or is it merely the neoliberal cop-out dressed in lavender lavender?
Kelly Gerrard January 3, 2026
This is exactly what needs to be said. No fluff. No excuses. If you're managing meds you owe it to your loved one to be meticulous. No more guessing. No more ‘I think it was yesterday’. Write it down. Check it. Ask. Period. This isn’t optional. It’s non-negotiable. Do it now.
Glendon Cone January 4, 2026
Just wanted to add-my grandma’s pharmacist gave us free stickers with the drug names and times printed on them. We stuck them right on the pill organizer. She still can’t read but she knows the colors now. Blue = morning, red = night. Simple. Brilliant. No app needed. Also, the QR codes? Life changer. My cousin scanned one and found out her dad’s ‘heart pill’ was actually an old thyroid med. That’s the kind of stuff that kills people. Thanks for the reminder to talk to the pharmacist. They’re the real MVPs.
Henry Ward January 5, 2026
Wow. Another ‘you’re not doing enough’ guilt trip disguised as helpful advice. I bet you’re the kind of person who judges people for using household spoons while you sip your $8 organic matcha latte. Not everyone has time, money, or a 24/7 caregiver. Maybe stop pretending this is about discipline and admit it’s about class. My aunt died because her meds were delayed by insurance bureaucracy-not because she forgot to write down ‘5 mg’.
Aayush Khandelwal January 6, 2026
Man, this whole thing is like a symphony of survival-polypharmacy as cacophony, pill organizers as metronomes, pharmacists as conductors. The real tragedy? We’ve turned human care into a checklist opera. But hey, at least we’re not using spoons anymore. Progress, baby. 🎻🩺
Sandeep Mishra January 8, 2026
Thank you for writing this with such heart. I’ve been mentoring new caregivers in my community and I share this exact guide every week. One thing I always add: if you’re overwhelmed, ask for help. Don’t carry it alone. There are support groups, free MTM sessions, even volunteer pharmacy aides in some cities. You’re not failing-you’re fighting. And you’re not alone. 🤝