Getting the medicine you need shouldn’t mean choosing between rent and refills. For millions of Americans, even with insurance, out-of-pocket costs for prescriptions can be overwhelming. High deductibles, formulary restrictions, and surprise price hikes make it hard to stay on treatment. That’s where patient advocacy foundations come in. These nonprofits don’t sell drugs or run insurance plans-they exist to make sure no one skips a dose because they can’t afford it.
What Are Patient Advocacy Foundations?
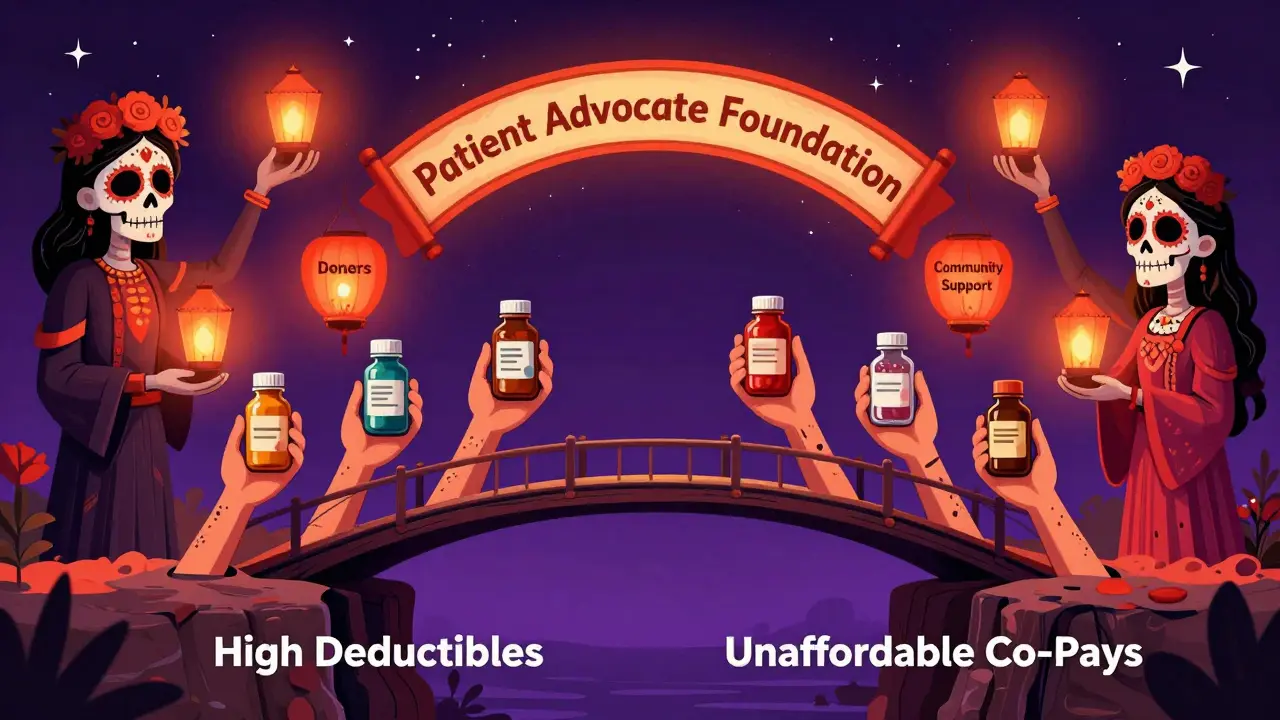
Patient advocacy foundations are nonprofit organizations that give direct financial help to people struggling to pay for medications. Unlike pharmaceutical company programs that only cover their own drugs, these foundations often support multiple conditions and can help with co-pays, deductibles, and even non-medical costs like transportation to appointments. One of the biggest and most trusted is the Patient Advocate Foundation (PAF) a national nonprofit established in 1996 that connects patients with financial aid, case management, and insurance navigation services. They don’t just hand out cash-they work with donors, pharmaceutical companies, and healthcare providers to fill gaps in the system.Who Qualifies for Medication Grants?
Eligibility isn’t one-size-fits-all. Each fund has its own rules, but most follow the same basic structure:- You must have a confirmed diagnosis of a serious, chronic, or life-threatening condition
- You’re currently in treatment, starting treatment within the next 60 days, or finished treatment in the last 6 months
- You’re a U.S. citizen or permanent resident receiving care in the U.S. or its territories
- You meet income guidelines (usually 500% of the federal poverty level or lower)
How PAF’s Co-Pay Relief Program Works
This is one of the most useful tools for insured patients. The Co-Pay Relief Program a PAF-managed initiative that provides financial assistance to insured patients for out-of-pocket medication costs covers co-pays, coinsurance, and deductibles for over 140 conditions-from cancer to rare autoimmune diseases. Here’s how it works:- You or your provider applies online at copays.org or calls 844-462-8072
- You submit proof of diagnosis, insurance card, and income documents (tax return, pay stubs, or a signed letter)
- Your doctor fills out a form confirming your treatment plan
- Once approved, the grant goes directly to your pharmacy or insurer-not to you
- You get a reduced co-pay at the counter, sometimes as low as $0
Other PAF Financial Aid Funds
PAF also runs condition-specific funds that go beyond co-pays. These help with things like:- Travel to treatment centers
- Home care services
- Specialized nutrition
- Medical equipment
- Sepsis/ARDS/TSS Fund: Requires diagnosis within the last 6 months, physician verification, and income under 500% of poverty level
- Thyroid Eye Disease Fund: Covers medications like Tepezza, which can cost over $100,000 per course
- Caregiver Support Fund: Supported by the American Cancer Society, helps with non-medical costs for cancer patients
How to Apply: Step-by-Step
Applying sounds complicated, but it’s simpler than you think. Here’s what to do:- Identify your condition and check if it’s covered on patientadvocate.org or copays.org
- Gather documents: Diagnosis letter from your doctor, insurance card, tax return or proof of income, and ID
- Call or apply online-don’t wait. Funds are first-come, first-served
- Get your provider to complete their part. Many applications stall because the doctor’s form isn’t submitted
- Track your status. You’ll get an email or call within 5-10 business days
- Reapply if needed. If your fund runs out, check back the first business day of next month
What Happens If the Fund Is Full?
This is the biggest frustration. Many funds are donor-funded and have a set budget. Once it’s gone, applications close-sometimes for weeks or months. For example, the Sepsis fund might run out by mid-January and reopen February 1st. That doesn’t mean you’re denied-it means you’re on a waiting list. You’ll get an email saying your application is pending. When funds return, they process applications in order. Don’t give up. Call the program monthly to check status. Some patients get approved after waiting 3-4 months.How PAF Compares to Other Options
There are other ways to get help-but each has limits:| Option | Best For | Limitations |
|---|---|---|
| Patient Advocate Foundation (PAF) | Insured patients with high co-pays, multiple medications, or rare conditions | Funds run out; not for uninsured patients needing full drug coverage |
| Pharmaceutical Company PAPs | Uninsured patients needing one specific drug | Only covers that company’s product; strict income limits; slow approval |
| Medicaid or Medicare Extra Help | Low-income seniors or disabled individuals | Requires enrollment in government program; long wait times |
| State Prescription Assistance Programs | Residents of states with public drug programs (e.g., NY, CA) | Varies by state; not available everywhere |
Common Mistakes to Avoid
People get turned down-not because they don’t qualify, but because they make simple errors:- Waiting until the last minute to apply-funds disappear fast
- Forgetting to get the doctor’s form signed
- Using outdated tax documents (must be from the last 12 months)
- Applying for the wrong fund (e.g., applying for cancer help when you have MS)
- Not checking back after a fund closes
What to Do If You’re Denied
If you’re denied, ask why. Sometimes it’s a paperwork error. Other times, your income is just above the limit-but you can still appeal. You can also:- Apply to other foundations like the HealthWell Foundation or the Chronic Disease Fund
- Ask your pharmacy about discount cards (GoodRx, SingleCare)
- Check if your drug has a generic version
- Contact your manufacturer’s PAP directly
Final Thoughts
You’re not alone. Over 28 million Americans are uninsured. Millions more are underinsured. Prescription costs keep rising-up 55% between 2014 and 2022. Patient advocacy foundations like PAF are not perfect, but they’re one of the few systems designed to protect people when the healthcare system fails them. Start with PAF. It’s free, confidential, and doesn’t require you to be perfect. Just be honest. Fill out the forms. Get your doctor’s help. Apply early. And if you get turned down, try again next month. Someone out there is paying for these grants so you don’t have to choose between your health and your rent.Can I get help if I have Medicare?
Yes. PAF’s Co-Pay Relief Program helps Medicare beneficiaries with Part D co-pays, but only if the medication is not covered by Medicare’s low-income subsidy program. If you’re already getting Extra Help, you may not qualify. Check with PAF directly-each case is reviewed individually.
Do I need to reapply every month?
No. Once approved, your grant typically lasts for the calendar year or until you reach the fund’s annual limit. But if your fund runs out mid-year, you’ll need to reapply when it reopens. Some programs cap annual assistance at $5,000 or $10,000, so plan ahead.
Can I apply for more than one fund at the same time?
Yes, if you have multiple qualifying conditions. For example, if you have cancer and diabetes, you can apply for both the Cancer Care Fund and the Diabetes Co-Pay Relief fund. Each application is separate, so make sure you meet the criteria for each one.
How long does it take to get approved?
Most applications are processed within 5 to 10 business days. If your doctor submits their form quickly and your documents are complete, you might get approved in 3 days. Delays usually happen when paperwork is missing or unclear.
What if I don’t have health insurance?
PAF’s Co-Pay Relief Program is only for insured patients. But you can still apply for PAF’s Financial Aid Funds, which help uninsured patients with treatment-related costs like travel, lab fees, or home care. You may also qualify for a pharmaceutical company’s free drug program-visit their website or call their patient support line.
Are these grants taxable?
No. Medication grants from nonprofit patient advocacy foundations are not considered income by the IRS. You won’t get a 1099 form, and you don’t need to report them on your taxes.
Can I get help for over-the-counter medications?
Generally, no. Most foundations only cover prescription drugs that are medically necessary and prescribed by a doctor. Over-the-counter medications like pain relievers or vitamins are not eligible unless they’re part of a specific, approved treatment plan (rare).
Is there a limit to how much help I can get?
Yes. Each fund has an annual cap, often between $5,000 and $15,000 per patient. Some programs cover 100% of your co-pay up to that limit. Others pay a fixed amount per month. The goal is to reduce your burden-not eliminate it entirely.








11 Comments
Annette Robinson January 7, 2026
I wish I’d known about this two years ago when my mom was struggling with her chemo co-pays. We were drowning in bills, and no one told us about PAF. She’s gone now, but I’m sharing this everywhere I can-no one should have to choose between medicine and groceries.
Aubrey Mallory January 9, 2026
This is the bare minimum. The system is broken. People shouldn’t need a nonprofit to survive their own treatment. Why are we letting pharmaceutical companies and insurance giants get away with this? It’s criminal. And we’re just sitting here thanking a charity instead of demanding change.
christy lianto January 10, 2026
Just applied for the Thyroid Eye Disease fund-Tepezza was going to cost me $120k out of pocket. I cried when I got the approval email. I didn’t think it was real. This isn’t charity-it’s justice. And if you’re reading this and you’re scared to apply? Do it anyway. The worst they can say is no. But if you don’t try? You’ll never know what you could’ve gotten.
Lois Li January 11, 2026
Thanks for laying this out so clearly. I’ve been helping my sister navigate this and honestly I was lost until I read this. The part about reapplying on the first of the month? That’s gold. I’m printing this out for her. Also, the doctor form thing-so many people miss that. I’ll remind her to call the office and beg them to submit it. Seriously, thank you.
Dave Old-Wolf January 13, 2026
So if I have Medicare, I can still get help? I thought they covered everything. Wait, no, I guess not. So this is like… extra help on top? And it’s not taxed? That’s good. I’m gonna look into this for my dad. He’s on insulin and it’s killing his budget.
Prakash Sharma January 14, 2026
Why does America even have this mess? In India, we have government-subsidized medicines for chronic diseases. People here are begging nonprofits just to breathe. This isn’t healthcare-it’s a lottery. And you’re lucky if you know the right words to say.
Donny Airlangga January 15, 2026
My cousin got approved for the Sepsis fund last year. She was in the ICU, couldn’t afford the antibiotics, and they told her to go home. She applied, got approved in 7 days, and lived. I didn’t even know this existed until she told me. I’m telling everyone I know now.
Kristina Felixita January 16, 2026
OMG, I just applied!! I’ve been stressing for months-my co-pay for my autoimmune med was $450!! I was gonna start splitting pills… I didn’t think anyone would help. And it’s FREE?? And not taxed?? I’m crying at my keyboard right now. Thank you thank you thank you!!
Evan Smith January 17, 2026
So… we’re praising a nonprofit for fixing a system that should’ve been fixed by Congress? Cool. Cool cool cool. I guess we should all just start a GoFundMe for our insulin instead of demanding universal coverage. Yeah, that’s the American way. 🙃
swati Thounaojam January 17, 2026
Applied last month. Got denied. Called them. They said my income was 2% over. I got a new pay stub. Reapplied. Got approved. Don’t give up.
Luke Crump January 18, 2026
Let me get this straight: we’ve created a society where a person’s survival depends on whether they can navigate a maze of nonprofit paperwork while dying? And we call this compassion? This isn’t help. This is the sound of civilization crumbling. The real tragedy isn’t the co-pay-it’s that we’ve normalized this.