When a drug can save lives but also cause serious harm - like birth defects, organ failure, or deadly blood disorders - how do you let patients get it without putting them at unacceptable risk? That’s the exact problem the FDA solved with REMS programs. These aren’t just paperwork. They’re legally required safety nets built into the system for some of the most dangerous medications on the market.
What Exactly Is a REMS Program?
REMS stands for Risk Evaluation and Mitigation Strategies. It’s a formal program the U.S. Food and Drug Administration (FDA) can force drug makers to put in place if a medicine has serious, life-threatening risks that standard warning labels can’t control. Think of it as a safety override: the drug is powerful enough to be approved, but only if extra steps are taken to make sure it’s used correctly.
REMS became official in 2007 under the Food and Drug Administration Amendments Act (FDAAA). Before that, the FDA had to improvise - like the strict controls on isotretinoin (Accutane) for acne, which could cause severe birth defects, or clozapine for schizophrenia, which can wipe out white blood cells. These early efforts laid the groundwork for today’s structured REMS system.
As of late 2024, there are about 120 active REMS programs covering 185 different drugs. That’s roughly 5.7% of all prescription medications in the U.S. - a small number, but they include some of the most critical treatments for cancer, multiple sclerosis, autoimmune diseases, and rare blood disorders.
The Three Core Parts of Every REMS
Not every REMS is the same, but they all include at least one of these three components. The most basic is the Medication Guide - a printed handout patients get with their prescription. It explains the risks in plain language, like what to watch for and when to call a doctor. About 78% of REMS programs require these guides.
The second layer is the Communication Plan. This targets doctors and pharmacists. It might be a letter from the drug company, a safety alert, or training materials. About 62% of REMS programs use this to make sure prescribers know exactly how to handle the drug safely. For example, a doctor prescribing thalidomide for leprosy or multiple myeloma must understand the extreme risk of fetal exposure and the mandatory pregnancy tests required.
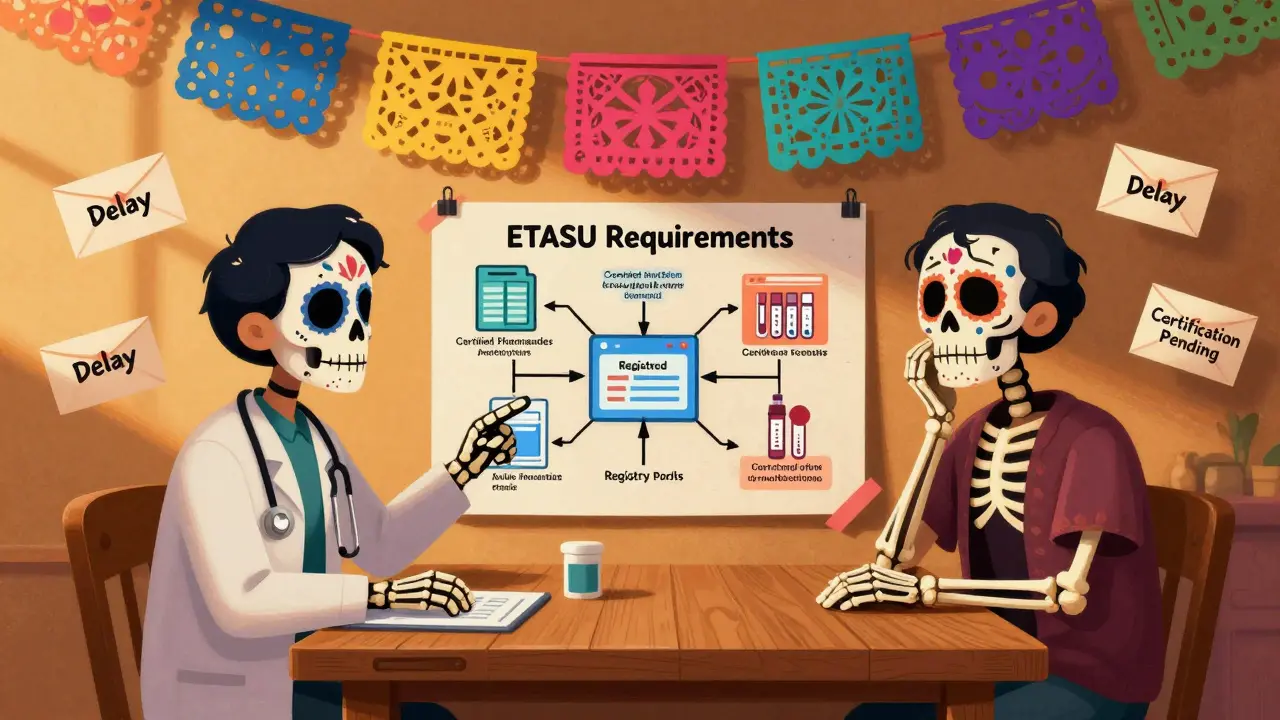
The most complex part is the Elements to Assure Safe Use, or ETASU. This is where things get heavy. About 45% of REMS programs include ETASU, and they’re the ones that cause the biggest headaches for providers and patients. ETASU can include:
- Prescriber certification - doctors must complete training and register to prescribe
- Pharmacy certification - only certain pharmacies can dispense the drug
- Restricted distribution - the drug can only be given in a hospital or specialty clinic
- Patient enrollment - patients must sign up in a registry to track outcomes
- Regular monitoring - blood tests, pregnancy tests, or imaging required before each dose
For example, the Revlimid REMS for multiple myeloma requires every prescriber to be certified, every patient to be enrolled in a registry, and women of childbearing age to have two negative pregnancy tests before each prescription. That’s not just a formality - it’s a process that takes time, paperwork, and coordination.
Who’s Responsible for Making REMS Work?
The drug manufacturer is legally on the hook. They have to design the REMS, train staff, distribute materials, and track results. The FDA gives them 120 days to submit a plan after deciding a REMS is needed. Once approved, they must submit annual reports proving the program is working. If it’s not, the FDA can demand changes - or even remove the REMS entirely. Only three REMS have been fully dropped since 2007, the most recent being Zeposia for multiple sclerosis in March 2023.
But the real work happens on the front lines. Doctors spend an average of 45 minutes per REMS program getting certified. Pharmacists spend extra time checking certification status, verifying patient enrollment, and logging data into online portals. One pharmacist on Reddit said the Entyvio REMS adds 15 to 20 minutes per prescription just for portal checks. That’s not a small delay - it’s a workflow breaker.
Specialty pharmacies handle 89% of REMS drugs because they’re the only ones equipped to manage the logistics. Regular pharmacies can’t handle the certifications, inventory controls, or documentation. So if your drug has a REMS, you’re likely getting it from a mail-order pharmacy, not your local CVS.
The Hidden Costs - For Patients and Providers
REMS programs cost money. A lot of it. The FDA estimates drug companies spend an average of $2.7 million per REMS program every year. That’s on top of research, manufacturing, and marketing. The total healthcare system cost? Around $1.2 billion annually.
But here’s the catch: those costs are justified. The FDA says REMS have prevented an estimated $8.4 billion in healthcare expenses by avoiding hospitalizations, emergency visits, and long-term complications from unsafe drug use.
Still, the burden on patients is real. A 2023 GoodRx survey found 42% of patients prescribed a REMS drug experienced delays in getting their medication. Why? Certification forms missing. Pregnancy tests not done on time. Specialty pharmacy approvals stalled. One patient with Lemtrada, a drug for multiple sclerosis, had to wait three weeks because the hospital needed to schedule a full infusion center review - all because of REMS rules.
For oncology practices, the problem is worse. The American Society of Hematology found that 68% of hematologists spend more than five hours a week just managing REMS paperwork for drugs like Revlimid and Pomalyst. That’s five hours not spent with patients - five hours lost to bureaucracy.
Why REMS Block Generic Drugs
There’s a dark side to REMS that’s rarely talked about: they’re being used to delay generic competition. In 2024, a study in Health Affairs found that 78% of generic drug makers reported delays of over 14 months just to get samples of the brand-name drug to test their version. Why? Because the brand company controls the REMS, and they can legally refuse to share samples unless the generic maker agrees to their terms.
This isn’t about safety - it’s about profit. The FDA has no authority to force companies to hand over samples. So even if a drug’s patent expired, the REMS becomes a legal barrier to cheaper alternatives. The 21st Century Cures Act Reauthorization of 2022 tried to fix this by requiring a 90-day review window for sample access, but enforcement is still weak.

What’s Changing in 2025 and Beyond
The FDA knows REMS are broken in places. That’s why they launched the REMS Modernization Initiative in 2023. The goal? Reduce paperwork without reducing safety. They’re working on:
- Standardizing forms across all REMS programs
- Building a national digital verification system so prescribers and pharmacists can check certification in seconds
- Creating a public REMS Dashboard by Q3 2025 that shows real-time data on how well each program is working
They’re also exploring how to use real-world data - like electronic health records and pharmacy claims - to monitor safety automatically instead of relying on manual checklists. Imagine a system that flags a patient who missed a blood test or a doctor who prescribed a drug without certification - all without human intervention.
Dr. Rachel Sherman, former FDA deputy commissioner, predicts REMS will soon be less about forms and more about data. “The future isn’t paper envelopes and online portals,” she said in a 2024 commentary. “It’s smart systems that know when a risk is real and when it’s just noise.”
Is REMS Working?
Yes - but not perfectly. REMS has kept thousands of patients safe from catastrophic harm. Without it, drugs like thalidomide or clozapine might never have been approved. The system works for its intended purpose: enabling access to high-risk, life-saving drugs while minimizing avoidable harm.
But it’s clunky, expensive, and uneven. A patient in New York might get their drug in two days. A patient in rural Kansas might wait three weeks because the nearest certified pharmacy is 150 miles away. A doctor in a small clinic might skip the certification because the paperwork is too much. That’s not safety - that’s access inequality.
The FDA’s next move will determine whether REMS becomes a modern, efficient tool - or stays a bureaucratic nightmare. If the 2025 REMS Assessment Standard delivers on its promise, we might finally see a system that protects patients without punishing providers or blocking affordable drugs.
For now, if you’re on a REMS drug, know this: the delays, the forms, the phone calls - they’re not there to make your life harder. They’re there because someone, somewhere, almost died from a drug that wasn’t handled right. And the system is trying, however imperfectly, to make sure that doesn’t happen again.
What drugs require a REMS program?
REMS programs apply to prescription drugs with serious safety risks that can’t be managed by standard labeling alone. Common examples include Revlimid (lenalidomide) and Pomalyst (pomalidomide) for multiple myeloma, Thalidomide for leprosy and cancer, Lemtrada (alemtuzumab) for multiple sclerosis, Clozapine for schizophrenia, and Isotretinoin for severe acne. As of 2024, about 185 drugs in the U.S. are covered by active REMS programs, mostly in oncology, neurology, and immunology.
Can I get a REMS drug from my local pharmacy?
Usually not. About 89% of REMS drugs require distribution through specialty pharmacies because they need special handling, certification tracking, and patient monitoring. Your local CVS or Walgreens likely doesn’t have the systems in place. You’ll typically get the medication by mail or through a hospital-based pharmacy. Your doctor or insurer will usually arrange this for you.
Why do I need to be certified to take a REMS drug?
You don’t need to be certified - your doctor and pharmacist do. Certification ensures they’ve been trained on the drug’s risks and how to manage them. For example, if you’re prescribed Revlimid, your doctor must complete a certification process to prove they understand the pregnancy risks and monitoring requirements. This protects you by making sure the person prescribing your drug knows exactly what could go wrong.
How long does a REMS program last?
REMS programs last as long as the FDA determines they’re needed. Manufacturers must submit annual reports proving the program is effective. If evidence shows the risks are now well-controlled - or if the program isn’t helping - the FDA can modify or remove it. Since 2007, only three REMS have been fully discontinued, showing how long-lasting these requirements can be.
Are REMS programs only in the U.S.?
Yes. REMS is a U.S.-specific regulatory tool created under the FDA Amendments Act of 2007. Other countries have different systems - like risk management plans in the European Union or safety monitoring programs in Canada - but none use the same structured, legally enforceable framework as the FDA’s REMS. The U.S. system is unique in its complexity and legal authority.
Can a REMS program be removed?
Yes, but it’s rare. The FDA can remove a REMS if data shows the benefits of the drug outweigh the risks without the extra safeguards. The most recent example was Zeposia (ozanimod) for multiple sclerosis, whose REMS was discontinued in March 2023 after years of monitoring showed no increase in serious side effects when used under standard labeling. Removal requires strong, long-term evidence - not just a few years of data.
What to Do If You’re on a REMS Drug
If your doctor prescribes a drug with a REMS, here’s what to expect and how to handle it:
- Ask your doctor for the name of the REMS program. Look it up on the FDA’s REMS@FDA website.
- Confirm your pharmacy is certified to dispense it. Don’t assume your local pharmacy can handle it.
- Keep track of required tests - pregnancy tests, blood work, or imaging - and schedule them ahead of time.
- Save all paperwork. Certification forms, enrollment confirmations, and lab results may be needed for refills.
- If you’re delayed, contact your doctor’s office or the drug manufacturer’s REMS support line. They often have dedicated staff to help.
REMS isn’t perfect. But it’s the best system we have to balance life-saving treatment with life-threatening risk. Understanding it helps you navigate it - and maybe even push back when it’s working against you instead of for you.







12 Comments
Linda Caldwell December 17, 2025
Been on Revlimid for 3 years now. The first time I had to get my pregnancy test done 3 days before my refill? I thought I was in the military. Now I just schedule it with my OB like a dentist appointment. It’s annoying but I’d rather be alive than angry.
BETH VON KAUFFMANN December 18, 2025
Let’s be real-REMS is just Big Pharma’s legal shield against generics. They don’t care about safety-they care about profit margins. The FDA’s ‘modernization’ is just a PR stunt while they let specialty pharmacies charge $20K/month for a drug that could be $200. This isn’t patient protection-it’s rent-seeking dressed up as bureaucracy.
Nishant Desae December 18, 2025
as someone from india where we dont have remss at all, i just cant believe how much paperwork you guys go through for one pill. here if a doctor prescribes something dangerous, they just say 'be careful' and hand you the bottle. no registry, no certification, no portal login. i mean... maybe its overkill? but then again, i read about the thalidomide babies and i get it. still, 45 minutes just to sign up? my uncle in delhi got his chemo without even a form. its wild.
Anna Giakoumakatou December 20, 2025
Oh wow. A government program that actually works? How quaint. I suppose next you’ll tell me the postal service still delivers mail on Sundays and that ‘safety’ isn’t just a marketing term invented by lawyers who hate innovation. The fact that you call this ‘necessary’ proves you’ve never met a real patient-or a real doctor. This isn’t medicine. It’s compliance theater with a side of corporate extortion.
Erik J December 21, 2025
I wonder how many REMS drugs are prescribed off-label without any of the required monitoring. Probably a lot. And yet, nobody gets caught. The system assumes compliance, but in practice, it’s just a checklist that gets ignored unless someone’s auditing. So is it really protecting anyone-or just creating the illusion of safety?
Anu radha December 22, 2025
my cousin in texas had to wait 2 weeks for her lemtrada because the pharmacy said the form was ‘incomplete.’ she cried. she was scared. she didn’t know what to do. i told her to call the drug company-they helped her in 2 hours. it’s not the system’s fault. it’s the people who don’t know how to use it.
Kaylee Esdale December 23, 2025
REMS feels like a parent who won’t let you drive until you’ve passed 17 tests-even though you’ve been riding bikes since you were 8. yeah, safety matters. but why does every single drug need its own weird app, its own portal, its own weird ritual? can’t we just build one system that talks to all the others? why are we still using PDFs in 2025?
Kent Peterson December 24, 2025
Let me get this straight-you’re proud of a system that forces American patients to wait weeks for life-saving meds while China and India just hand out pills like candy? This isn’t safety, it’s weakness. We’re so obsessed with avoiding every possible risk that we’re killing people with delays. If you can’t handle a little responsibility, maybe you shouldn’t be on the drug at all. Stop outsourcing your accountability to a government form.
Pawan Chaudhary December 24, 2025
just wanted to say thanks to the folks who built this system. i know it’s a pain, but my sister’s on clozapine and she’s been stable for 5 years. no hospital stays. no ER visits. just quiet, steady life. that’s worth the paperwork. i’ll fill out 100 forms if it keeps her safe.
Evelyn Vélez Mejía December 25, 2025
REMS is not a policy-it’s a moral artifact. It is the institutional embodiment of our collective guilt: the fear that if we do not overregulate, we will become the architects of another thalidomide. And yet, in our zeal to prevent the unthinkable, we have built a labyrinth that punishes the very people it claims to save. Is safety the absence of risk-or the presence of dignity? The system answers with forms. The patient answers with silence.
Meghan O'Shaughnessy December 25, 2025
as a nurse in rural oregon, i’ve seen patients drive 3 hours just to get a REMS drug because the nearest certified pharmacy is 150 miles away. one woman missed her dose for 6 weeks because her car broke down. she was scared. she didn’t know what to do. we need mobile clinics. we need tele-certification. we need to stop treating rural patients like they’re a footnote in a regulatory manual.
Michael Whitaker December 26, 2025
As a former FDA contractor, I must say: the REMS Modernization Initiative is a noble idea-but it’s being sabotaged by legacy IT vendors who profit from the current chaos. The FDA doesn’t lack vision; it lacks teeth. The system is designed to be inefficient because someone’s making millions off the paperwork. And until Congress forces a real audit of these vendor contracts, nothing will change. I’ve seen the reports. The data is there. The will? Not so much.